-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Referrals
- Referral Forms/Contact
- Direct Connect
- Referring Veterinarian Portal
- Clinical Articles
- Partners in Care Newsletter
CE, Internships & Alumni Info
CE Seminar Schedule
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 By Zachary Crouse, DVM, DACVIM (SAIM)
By Zachary Crouse, DVM, DACVIM (SAIM)
angell.org/internalmedicine
internalmedicine@angell.org
617-541-5186
Intraluminal tracheal stenting provides a minimally invasive, non-surgical method for the treatment of a narrow or obstructed tracheal lumen. Tracheal stenting can be used for the treatment of tracheal stricture, tumors, and collapse.1 Prior to recommending tracheal stenting, it is important to understand the indications, limitations, and complications of this palliative procedure. Client education and regularly scheduled follow up appointments are essential to successful outcome and management.
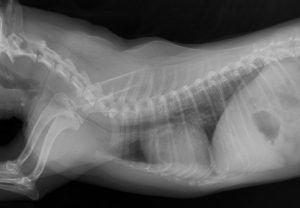
Tracheal collapse is the most common indication for tracheal stenting. Tracheal collapse most commonly affects middle-aged to geriatric small and toy breed dogs.2 It results from weakening of the tracheal cartilage, leading to dorsoventral flattening of the trachea and laxity of the dorsal tracheal membrane, and can affect the cervical or intrathoracic trachea.2,3 A majority of dogs with tracheal collapse will respond well to medical management for a period of greater than 12 months.3 Medical management typically involves a combination of antitussives, anti-inflammatories, and bronchodilators and must be tailored to each patient.1 Appropriate candidates for tracheal stenting include dogs with tracheal collapse that have failed aggressive medical management despite appropriate therapy for any identified comorbidities, dogs that present with life-threatening upper airway obstruction secondary to tracheal collapse and do not respond to conservative therapy, and dogs and cats with tracheal strictures or tumors.1, 3, 4
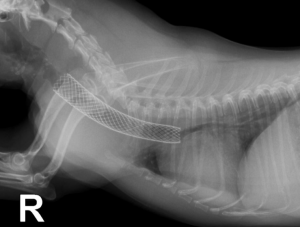
Current iterations of veterinary tracheal stents are made of a self-expanding, nitinol mesh.1,3 Patients are placed under general anesthesia and intubated for the procedure. A combination of tracheobronchoscopy and fluoroscopy is used to identify the location of the tracheal collapse and to measure the tracheal size. Tracheal stents are typically oversized by 2-3 mm, compared to the size of the expanded trachea, in order to minimize future foreshortening and migration.1 The tracheal stent is opened slowly under fluoroscopic guidance to ensure appropriate placement, and the patient is extubated in the process. Repeat tracheoscopy is used to confirm that the stent has opened fully and post-operative radiographs are obtained to document the stent location.1 The patient is recovered in the critical care unit and is discharged, typically the following day, on antitussives, prednisone, and antibiotics.
While reports of tracheal stenting for treatment of stricture and tumors are limited, there is a growing knowledge base surrounding the use of tracheal stents for treatment of tracheal collapse. Studies have shown that a large majority of clients are satisfied with the results of the procedure and that most dogs display improvement of their clinical signs (75-90%).3,5 The subset of patients with raspy breathing and honking respond best to tracheal stenting, while the outcome of those with coughing as their primary sign is more difficult to predict.1 Dogs with mainstem bronchial collapse are likely to have persistent coughing after tracheal stenting.1 One study found that mean survival time in dogs treated for tracheal collapse with either tracheal stent or extraluminal tracheal rings was significantly shorter in dogs with bronchial collapse versus those without bronchial collapse (325 days vs. 1,600 days).6 Despite the shorter mean survival time, many of these dogs with bronchial collapse will respond well to tracheal stenting as it can still improve airflow and reduce dyspnea.1
Periprocedural morbidity and mortality are low with tracheal stenting, with one study reporting 11% mortality within 60 days of stent placement.5 There are, however, several long term complications associated with tracheal stenting of which clients should be aware. Foreshortening occurs in over 80% of cases, but is often not clinically relevant.1,5 Migration of the stent may occur if it was undersized at the time of placement.1 Stent fractures have been reported in 10-42% of cases, depending on the type of stent used, however this number is likely to decrease with time as tracheal stent materials and design continue to improve.1,7 Stent fractures can typically be stabilized by placement of a second tracheal stent within the lumen of the first, extending cranially and caudally to the point of fracture.3 Inflammatory or granulation tissue ingrowth into the lumen of the stent occurs in about one third of cases.5 In many cases, this tissue ingrowth will respond to anti-inflammatory doses of prednisone, suggesting that these lesions are primarily inflammatory in nature.7 Bacterial tracheitis or pneumonia can occur in dogs with tracheal stents, and should be considered when acute worsening of clinical signs is observed.1,7
After placement of a tracheal stent, almost all patients will still require medical management.1 This most commonly consists of antitussives, but can also include bronchodilators and anti-inflammatories. It is important to stress to clients that medication administration in these patients will be lifelong. Additionally, patients should present to the hospital every 3-6 months for a physical exam and thoracic radiographs. Any worsening of clinical signs should be investigated aggressively, as delay in treatment of tracheal stent complications can be devastating.
Tracheal stenting is a valuable tool in the treatment of tracheal disease, particularly tracheal collapse. As veterinary knowledge and experience grows and stent design continues to advance, outcomes with tracheal stenting will continue to improve. Careful patient selection, client education, and regularly scheduled monitoring are vital to achieving good outcomes.
References
- Weisse C. Intraluminal tracheal stenting. In: Veterinary image-guided interventions. 1st edn, Weisse C and Berent A eds, Wiley Blackwell, Ames, IA. 2015:73-82.
- Maggiore AD. Tracheal and airway collapse in dogs. Vet Clin North Am Small Anim Pract. 2014 Jan; 44(1):117-27.
- Tappin SW. Canine tracheal collapse. J Small Anim Pract. 2016 Jan; 57(1):9-17.
- Beal MW. Tracheal stent placement for the emergency management of tracheal collapse in dogs. Top Companion Anim Med. 2013 Aug; 28(3):106-11.
- Durant AM, Sura P, Rohrbach B, and Bohling MW. Use of nitinol stents for end-stage tracheal collapse in dogs. Vet Surg. 2012 Oct; 41(7):807-17.
- Tinga S, Thieman Mankin KM, Pycke LE, and Cohen ND. Comparison of outcome after use of extra-luminal rings and intra-luminal stents for treatment of tracheal collapse in dogs. Vet Surg. 2015 Oct; 44(7): 858-65.
- Weisse C. Insights in tracheobronchial stenting and a theory of bronchial compression. J Small Anim Pract. 2014 Apr; 55(4):181-4.