-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 By Martin Coster, DVM, MS, DACVO
By Martin Coster, DVM, MS, DACVO![]()
angell.org/eyes
ophthalmology@angell.org
617-522-7282
January 2021
This article shares some tips and tricks for performing successful eye exams.
1. It’s all in the holder
The key to performing a decent eye exam is to have the animal restrained appropriately, which may take one or two (and sometimes even three) assistants. The pet’s eyes should be at the examiner’s eye level, which means in most cases the pet should be on an exam table, with the examiner seated at a good height to make eye-to-eye contact without sacrificing ergonomics. An adjusting stool and/or table will therefore be needed. The pet’s head should be restrained with one hand under the chin and one at the back of the skull. This means a second holder may be needed to control the body if the patient will not stay still. A third assistant may be needed to open the eyelids or control front legs. Pre-visit sedation or anti-anxiety medications to facilitate a less-stressed, less fearful visit can be very helpful to performing a complete eye exam.1,2
2. Darkness is key
The ideal examination room is one in which external light sources (windows, doors, and even light seeping in around doors) can be completely blocked out. An easily-accessible dimmer switch on the room lights can help greatly to allow the eye exam to be performed at varying levels of light intensity. A red light can be used to provide working illumination. This reduces incidental light reflections on the surface of the eye, which maximizes the examiner’s ability to look into the eye with direct illumination.

Figure 1: Ophthalmology examination room; note blacked-out window on the door, red light, and adjustable stools. In this setup, the main room lighting is controlled by a dimmer switch easily accessible under the examination table.
3. Don’t forget the basic tests
Performing Schirmer tear test, fluorescein stain, and intraocular pressure are essential tests in order to make a diagnosis. Dry eye in particular is often overlooked for lack of a tear test, the normal value of which is 15mm/min or greater, in the absence of clinical signs. Intraocular pressure should be interpreted in light of other exam findings. For example, although a normal pressure of approximately 15mmHg is expected, this may be considered glaucomatous in a case of severe uveitis. As a variety of Icare® TONOVETs have become increasingly popular due to ease of use compared with the Tono-Pen®, knowing the normal values for your instrument is important. For example, the TONOVET Plus may read around 4 to 5 mmHg higher than the standard TONOVET, although the TONOVET Plus may be providing a truer pressure measurement.3

Figure 2: Three generations of tonometers; the Reichert Tono-Pen® XL; the TONOVET®; the Icare® TONOVET Plus. The Schiotz tonometer is not pictured as it has been consigned to our time capsule.
4. Follow an ordered exam
A thorough eye exam should have an ordered approach that is consistent every time. This maximizes the chance that every structure will be looked at and thus all conditions can be diagnosed. An “outside-in” approach is most common, assessing global vision and pupillary light reflex assessments, facial conformation and orbit, eyelids including third eyelid, conjunctiva, cornea, anterior chamber, iris, lens, vitreous, and retinal exam. Most practices do not have a slitlamp biomicroscope as used by ophthalmologists. Therefore, the magnification provided by a headloupe is very helpful, and having a well-charged bright transilluminator can make a huge difference over a dimmer light source. An ophthalmoscope can be used with its slitbeam for further anterior chamber assessment. Fundic examination is best performed with an indirect lens (20 or 28 diopter) and bright transilluminator.
5. Prescribe out when necessary
Many veterinarians are unable to carry numerous ophthalmic medications in their pharmacy. Fortunately, most ophthalmic drugs are also used in humans, and thus do not all need to be stocked in-house. This may sound like a simple tip, but all too often we see referral patients in whom a correct diagnosis was made but appropriate medications were not prescribed due to “lack” of availability.
6. Drugs that penetrate into the eye
Not all topical drugs penetrate through an intact corneal epithelium. For antibiotics, choices are limited to fluoroquinolones (e.g. ofloxacin and ciprofloxacin) or chloramphenicol. Non-steroidal anti-inflammatory drugs (NSAIDs, e.g. diclofenac, flurbiprofen, and ketorolac) and of course all glaucoma drops penetrate into the eye, but only certain steroid salts will penetrate. These are prednisolone acetate and the dexamethasone found in neo-poly-dexamethasone; in this latter case, solution may penetrate better than ointment. Antibiotics, NSAIDs, and steroids will not penetrate much deeper than the aqueous humor, and so posterior segment disease must be treated with systemic medications.
7. Neo-Poly-Hydrocortisone is rarely used by this author
This steroid does not penetrate into the eye so cannot treat uveitis, and is rarely strong enough for ocular surface inflammation. Its use is thus quite limited. Allergic inflammation might respond but may do better with specific antihistamine eye drops such as patanol or ketotifen.
8. Never underestimate pain
Clients frequently report their pet is comfortable, while also reporting the animal squinting at home. A careful history can elucidate other symptoms of pain, such as reduced appetite or altered behavior, or rubbing at the eye or face. Whether treating corneal ulcers, conjunctivitis, glaucoma, or uveitis, pain control should not be overlooked. Topical anesthesia (e.g. proparacaine) is inappropriate except for diagnostics, due to potential epithelial toxicity. Systemic pain control with an oral NSAID, gabapentin, fentanyl patch, and/or injectable/oral opioids should be considered as indicated.
9. Sclerosis vs. Cataract
One of the hardest determinations to make is whether an eye has cataract versus lenticular a.k.a. nuclear sclerosis (complicated even further when both are present). Generally, nuclear sclerosis should not occur in an animal younger than 7-8 years of age, and should be bilaterally symmetrical when present. Iatrogenic dilation with tropicamide or dark room examination with a relatively dim (so as not to elicit the pupillary light reflex) direct light source may be needed to visualize the perimeter of the lens. Dense nuclear sclerosis can obscure the fundus and behave like a cataract, but generally the fundus should be easily visualized even through sclerosis. The outer cortex should be clear with sclerosis. True cataract can be bilaterally symmetrical, but is rarely homogenous throughout the lens, and obscures fundic examination.

Figure 3: Nuclear sclerosis a.k.a. lenticular sclerosis, in the left eye of a dog; note the pearlescent central (nuclear) opacity. This opacity should be in symmetry with the other eye. This eye is iatrogenically dilated with tropicamide.
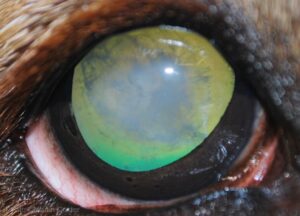
Figure 4: Nuclear cataract, in the right eye of a dog. Note the dense, heterogeneous white opacity obscuring the central view of the yellow/green tapetal reflection.
10. Tips for a fundic exam
The retinal exam is the hardest part of an eye exam and is thus often unfortunately overlooked or skipped entirely. Iatrogenic dilation with tropicamide (assuming intraocular pressure is normal and glaucoma or lens luxation are not suspected) is extremely important for a full retinal exam; however the time limitations of private practice, and owner constraints on time, can often preclude this. In these instances, dark room examination using a slightly dimmer light source and a 28 diopter lens (as opposed to a 20 diopter lens used for dilated exams) can provide visualization through a mid-range pupil. Once again, it is essential to have a trained assistant or two, to restrain the patient and hold open the eyelids as needed. Standing arms distance away from the eye, bring a transilluminator up close to the patient’s eye, obtain a tapetal reflection and then bring the light source back to the level of your own eye, still directed at the fundus. At this point, bring an indirect lens into alignment with the light and patient’s eye, close enough to the eye that you can observe the iris and pupil. Once the pupil is centered in the lens, bring the lens closer to you until it is about a finger’s length away from the eye (stabilize your hand by extending a finger to touch the side of the face or bridge of the nose). If you lose the view of the fundus, or to alter position, swing the lens away, re-gain the tapetal reflection, and swing the lens back into place.
Footnotes & References
- In an abstract presented at the 49th Annual Scientific Meeting Of The American College Of Veterinary Ophthalmologists, Minneapolis, Minnesota, Sept 26‐29, 2018, titled “Effects of oral trazodone on canine tear production and intraocular pressure” Pelych et al concluded that “administration of 5 or 9 mg/kg of trazodone does not significantly affect tear production or IOP in dogs within 6 hours”.
- If used for pre-visit sedation, gabapentin might lower intraocular pressure in the dog, but not a clinically significant amount; however its effect on glaucoma have not been studied: Shukla AK, Pinard CL, Flynn BL, Bauman CA. Effects of orally administered gabapentin, tramadol, and meloxicam on ocular variables in healthy dogs. Am J Vet Res. 2020 Dec;81(12):973-984. doi: 10.2460/ajvr.81.12.973. PMID: 33251843.
- Minella AL, Kiland JA, Gloe S, McLellan GJ. Validation and comparison of four handheld tonometers in normal ex vivo canine eyes. Vet Ophthalmol. 2020 Jun 1. doi: 10.1111/vop.12780. Epub ahead of print. PMID: 32478941.