-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Referrals
- Referral Forms/Contact
- Direct Connect
- Referring Veterinarian Portal
- Clinical Articles
- Partners in Care Newsletter
CE, Internships & Alumni Info
CE Seminar Schedule
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now

avianexotic@angell.org
617-989-1561
The most common presentation for rabbits through our busy emergency service is change in appetite. Most owners are aware that rabbits should be steadily eating and defecating throughout the day. When these habits change, either acutely or over several days, evaluation by a veterinarian is warranted. Early differentiation between gastrointestinal stasis and gastrointestinal (GI) obstruction is crucial and changes the treatment plan and prognosis. A systematic approach to an anorexic rabbit allows for an earlier diagnosis and appropriate case management.
Rabbits are monogastric hind-gut fermenters that have specific dietary requirements for normal dental and gastrointestinal health. Wild rabbits are considered browsers, as they are selective in what they ingest. Their digestive anatomy and physiology allow for efficient digestion and nutrient extraction from a high-fiber diet with low gut fill compared to grazers like cattle. This is in part due to the expulsion of high-fiber fecal content and packaging of nutrient dense cecotropes for reingestion.
Gastrointestinal stasis acts as an umbrella term for decreased appetite or fecal production. This syndrome can also be described as ileus, since gastrointestinal contractions have slowed or diminished. Owners will report that fecal pellets are smaller, dryer, or fewer in number over several days. Appetite may also be diminished, and some patients will only accept treats or their favorite food items. A variety of underlying causes can contribute to the symptoms displayed, and these different etiologies will alter the treatment plan implemented. Diet, underlying health condition, pain, or stress can all contribute to the onset of gastrointestinal stasis. A thorough history of the signs displayed prior to presentation as well as the husbandry provided at home will offer clues.
Diet is often one of the largest contributing factors to gastrointestinal stasis. Rabbits provided with unlimited hay, making up more than 50% of their diet, will consume an appropriate amount of indigestible fiber. This fiber plays an important role in gut motility and transit time by stimulating peristalsis throughout the GI tract. Rabbits unintentionally consume hair through grooming, but unlike other animals, they lack the ability to vomit hair balls back up. This is inability to vomit is due to a narrow cardiac sphincter in the stomach. As a result, the movement of hair through the gastrointestinal tract relies on continuous peristaltic contractions. A diet lacking fiber allows for excessive hair to build up in the stomach, which results in anorexia. Dehydration of the gastric contents develops, followed by eventual discomfort that further contributes to hypomotility. Indigestible fiber also plays an important role in the sorting and transfer of soluble (digestible) fiber at the ileocecocolic junction. Diets low in fiber can also result in cecal dysbiosis, or the disruption of the delicate balance of organisms within the rabbit’s digestive tract. The cecum acts as a large fermentation vat composed of many types of anaerobic organisms, such as Bacteroides species, gram-negative oval and fusiform rods, amoeba, and protozoa. The cecum also harbors a species of Sarcomyces yeast (Cyniclomyces guttulatus) in low numbers under normal circumstances. One of the most common ways that owners unknowingly contribute to cecal dysbiosis is by feeding rabbits food items that are too high in simple sugars and starches. These diets typically also have reduced fiber content, which results in cecocolic hypomotility. When the normal flora population is exposed to carbohydrates for long periods of time, excessive fermentation occurs, and the populations of organisms shift. Yeast proliferate, and the typically low numbers of Escherichia coli and Clostridium species begin to multiply, resulting in soft stool or in severe cases, true diarrhea. The excess glucose allows Clostridium to create iota-toxin, which can result in enterotoxemia and death.
Gastrointestinal stasis can also be triggered by episodes of excessive stress. As a prey species, rabbits have the potential to be susceptible to changes in the patient’s home or normal routine. This can be something as simple as a visitor to the household, addition of a new pet or family member, a sudden change in food, loud noises or other environmental changes, or travel (such a car ride). Each individual may to respond to these events differently. Any underlying health issues can also contribute to the onset of anorexia that may result in gastrointestinal stasis. Health issues such as dental disease, respiratory infection, Encephalitazoon cuniculi, urinary tract disease, or liver lobe torsion all have the potential to result in gastrointestinal stasis.
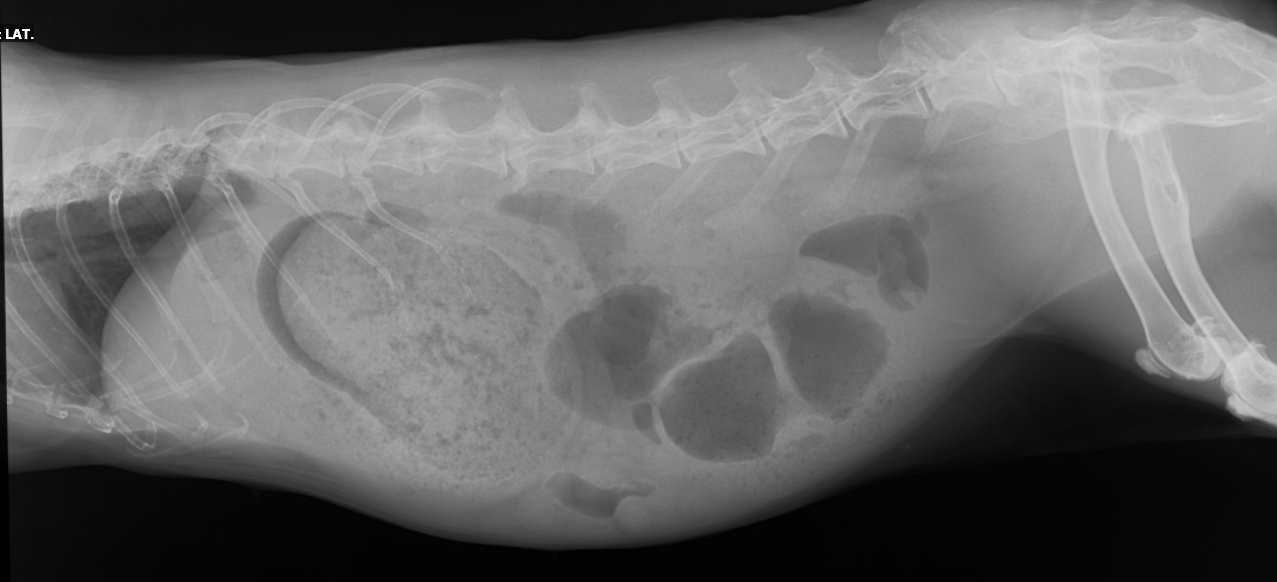
A thorough physical exam and diagnostic plan will allow a clinician to determine the underlying issue and provide appropriate treatment. However, an underlying cause is often not determined, yet patients will still respond to proper supportive care. Full-body radiographs, a complete blood count, and a chemistry panel are always recommended as a baseline workup for these patients. Radiographs often show granular material within the stomach and a gas halo outlining the ingesta (Figure 1). A variable amount of gas may accumulate throughout the intestines and cecum as fermentation continues in the absence of peristalsis. Mainstays of treatment include subcutaneous fluid therapy, analgesia, assisted feeding, and prokinetic medications. Deciding whether these patients are treated on an outpatient basis varies with the severity of clinical signs and lab results.
Gastrointestinal obstruction often has a more acute presentation than GI stasis. Owners report that their rabbit was normal earlier in the day but now seems uncomfortable and refuses to eat. The rabbit may also abruptly stop defecating. The most common site of obstruction is within the proximal duodenum due to a sharp turn of the pyloric outflow tract at the cranial duodenal flexure and subsequent narrowing of the duodenum. Another common site of obstruction is the ileocecocolic junction, where the fiber sorting occurs. The intestinal lumen narrows here as well. The most common cause of obstruction is a felted matt of rabbit fur that has been ingested from grooming. Carpet fibers, towels, and plastic can also cause obstruction. Similar to other species that have gastrointestinal obstruction, profound electrolyte abnormalities can occur, so rabbits may present as dull or obtunded. Acute gastric rupture is possible, which can result in sudden death.
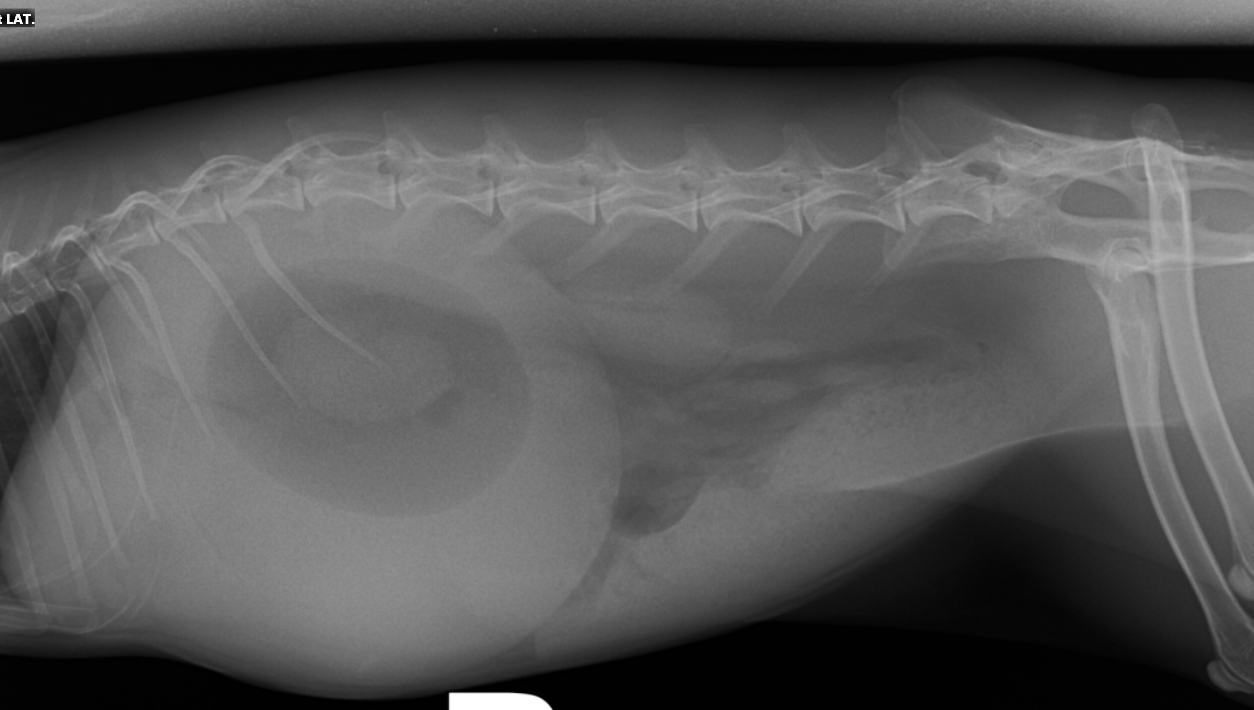
When a rabbit is triaged by the emergency service for decreased appetite, one of the most important early vital signs is body temperature. All hypothermic rabbits are provided with immediate heat support using heated blankets, heated discs, incubators, or forced-air blankets. Patients presenting with gastrointestinal stasis have a normal core temperature or mild hypothermia (98-101°F). Rabbits suffering from GI obstruction may be in hypovolemic or decompensatory shock, and are often profoundly hypothermic (<98°F). Aggressive heat support is provided prior to any further diagnostics, as stress can result in cardiopulmonary arrest. Once normothermic, a brief physical exam usually reveals a distended, turgid stomach. These patients are typically painful during palpation. Analgesia is provided and radiographs obtained. In the case of proximal duodenal obstruction, the stomach will be moderately to severely enlarged with fluid and have a central gas bubble of varying size (Figure 2). If the obstruction is farther downstream or at the ileocecocolic junction, then loops of intestines upstream of the obstruction will be distended with fluid and gas. These patients need aggressive intravenous fluid support starting with a shock bolus of fluids to correct blood pressure, followed by twice maintenance fluids if the patient can support it (e.g., no known heart condition, etc.). A complete blood count and chemistry panel should always be submitted, as electrolyte abnormalities may need to be addressed. Confirming hyperglycemia, often greater than 400mg/dl, further supports a diagnosis of obstruction, as glucose is often normal to mildly elevated in cases of GI stasis. Rehydrating the gastrointestinal tract will sometimes allow for the obstruction to pass. If the stomach is severely distended, decompression with an orogastric tube can relieve some pressure on the outflow obstruction and improve the comfort of the patient. Patients are provided access to food and water, but no oral treatments are administered. Resolution of the obstruction is sometimes obvious, as the patient will no longer require heat support, will start eating, and will begin producing feces again. Repeating radiographs is recommended if improvement is ambiguous. Surgical treatment is reserved as a last resort for patients who fail medical management. Surgical prognosis is guarded, but varies from case to case.
While rabbits presenting with gastrointestinal stasis or gastrointestinal obstruction can present with similar histories and clinical signs, prompt differentiation is important so that the most appropriate treatment plan can be implemented.
References
- Campbell-Ward ML. Gastrointestinal Physiology and Nutrition. In Quesenberry K, Carpenter J (eds): Ferrets, Rabbits, and Rodents: Clinical Medicine and Surgery, 3rd ed. St. Louis: Elsevier, 2012, P 183-191.
- Oglesbee BL, Jenkins JR. Gastrointestinal Diseases. In Quesenberry K, Carpenter J (eds): Ferrets, Rabbits, and Rodents: Clinical Medicine and Surgery, 3rd ed. St. Louis: Elsevier, 2012, P 193-197.
- Lichtenberger, Marla. “Fluid Resuscitation and Nutritional Support in Rabbits with Gastric Stasis or Gastrointestinal Obstruction.” Exotic DVM. Volume 7. Issue 2 (2005): 34-39.
- Harcourt- Brown FM, Harcourt-Brown SF. “Clinical Value of Blood Glucose Measurement in Pet Rabbits.” The Veterinary Record. Volume 170. Issue 26 (2012): 674.