-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Referrals
- Referral Forms/Contact
- Direct Connect
- Referring Veterinarian Portal
- Clinical Articles
- Partners in Care Newsletter
CE, Internships & Alumni Info
CE Seminar Schedule
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 By Maureen Carroll, DVM, DACVIM
By Maureen Carroll, DVM, DACVIM ![]()
angell.org/internalmedicine
internalmedicine@angell.org
617-541-5186
May 2022
Hyperlipidemia is defined as an increase in plasma triglycerides and/or cholesterol. It results from a disturbance in plasma lipoprotein metabolism. The increase in plasma lipids or lipoproteins may be due to accelerated synthesis or delayed degradation. An increase in plasma lipids in the fasted state is considered abnormal; however, the decision to treat should be based on repeatability and the magnitude of the increase. The following will detail the basic physiology behind lipid metabolism, hyperlipidemia conditions, and current treatment recommendations.
To begin, the biologically essential lipids are outlined below:
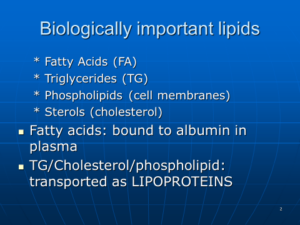
Lipid Metabolism Overview
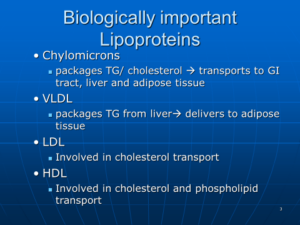
Due to the insoluble nature of free cholesterol and triglycerides, transport requires incorporation into various lipoproteins. The lipoproteins are arranged such that the polar regions (apolipoproteins, phospholipids, cholesterol) are on the outside, and the nonpolar regions (triglycerides and cholesterol- esters) are in the inner core. The apolipoproteins on the outer surface are responsible for the structure of the lipoprotein particle, the binding of the particles to the cell surface receptors, and the activation of various enzymes. Lipoproteins are classified based on size, density, electrophoretic mobility, and the concentrations of cholesterol and/or triglycerides.
There are four major classes of lipoproteins: 1. Chylomicrons 2. Very low-density lipoproteins (VLDL) 3. Low-density lipoproteins (LDL), and 4. High-density lipoproteins (HDL). Chylomicrons and VLDLs are primarily involved in triglyceride metabolism and transport. In contrast, LDCs and HDLs are involved mostly in cholesterol metabolism and transport.
Apolipoproteins influence the function of various lipoproteins. For example, apolipoprotein A-1 (apoA1) is HDL’s primary structural protein component. Apolipoprotein A-4 (apoA4) is present in chylomicrons and VLDL. It acts primarily in reverse cholesterol transport (see below) and intestinal lipid absorption via chylomicron assembly and secretion. Apolipoprotein C-3 (apoC3) plays a vital role in lipid metabolism, specifically regulating the metabolism of triglyceride-rich lipoproteins (chylomicrons and VLDL). Apolipoprotein B (apoB) plays an essential role in lipoprotein transport and is the primary organizing protein of many lipoproteins. Finally, apolipoprotein E (apoE) is involved in the transport and uptake of cholesterol by way of its affinity for lipoprotein receptors, including the LDL receptor.
Chylomicrons transport triglycerides and cholesterol through the lymphatics and plasma to the liver and adipose tissue. They are present in plasma 30 minutes to two hours after consuming a fat-containing meal. High levels of lipoprotein lipase (LPL) are found near the endothelial cells of both adipose and muscle tissue. Once LPL is activated, chylomicrons are hydrolyzed to free fatty acids and glycerol within 6 to 10 hours. The FFA’s diffuse into cells and are either used for energy or stored as triglycerides in adipocytes. The chylomicron remnant remains in the plasma until removed by the liver. Of note, lipoprotein lipase is under positive feedback control by insulin.
Excess fatty acids not used for energy are re-synthesized into triglycerides and packaged as VLDL. The formation of VLDLs is important in removing excess fatty acids from plasma and aids in mobilizing it for storage elsewhere. Lipoprotein lipase hydrolyzes the triglyceride (note: a triglyceride is a glycerol molecule with three fatty acids attached) portion of VLDL into free fatty acids and glycerol, supplying cellular needs of fatty acids. The liver then takes up the VLDL remnant via a specific receptor-mediated mechanism. This is a very efficient process in dogs, decreasing the time in circulation for VLDLs and their remnants. This is offered as one explanation for why dogs can eat higher-fat diets without developing coronary artery disease.
Removal of triglycerides, phospholipids, and apolipoproteins (C, E) from VLDL and the addition of apoB100 creates the cholesterol-ester-rich LDL. This molecule transports cholesterol to tissues for use in cell membrane synthesis and steroid hormone production. Although LDL and VLDL use the same receptor for removal from circulation, the efficiency of LDL removal appears to be less than that of VLDLs. Canine LDL is higher in triglycerides and contains less cholesterol than human LDL.
HDL is synthesized in the liver and secreted into circulation. Plasma lecithin-cholesterol acyltransferase (LCAT) esterifies cholesterol to hydrophobic cholesterol esters. This moves the esters from the outer surface to the inner core of the molecule, creating a concentration gradient such that excess tissue cholesterol is transferred to the HDL molecule. The excess cholesterol is then carried to the liver for excretion in bile. This process is known as reverse cholesterol transport and why HDL is called the ‘good cholesterol.’ Cats appear to lack LCAT and accomplish reverse cholesterol transport by direct tissue uptake of cholesterol esters.
Hormone-sensitive lipase (HSL) is another key enzyme that aids in the endogenous mobilization of lipids. Unlike lipoprotein lipase, HSL is under negative feedback control by insulin. Levels of this hormone are increased during states of poor nutrition and the presence of increased ACTH, corticosteroids, growth hormone, hyperthyroidism, and states of increased glucagon: insulin activity such as diabetes and pancreatitis.
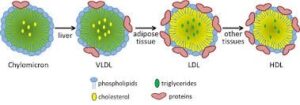
Image from Lipoproteins/Study.com
Hyperlipidemia Disorders
Hyperlipidemia refers to an increased concentration of triglycerides, cholesterol, or both in the blood. Lipid metabolism has two main pathways exogenous pathway and the endogenous pathway. The exogenous pathways are associated with the metabolism of dietary lipids. Post-prandial hyperlipidemia, mainly due to increased chylomicron concentration, is the most common cause of increased serum TG levels. This is considered normal and usually resolves in 2-10 hours. Cholesterol concentrations in patients with post-prandial hyperlipidemia are usually normal or only mildly increased. The endogenous pathway is associated with the metabolism of endogenously produced lipids, namely VLDL, LDL, and HDL.
Hyperlipidemia can be primary or secondary. Primary hyperlipidemia is usually breed associated and observed in such breeds as Miniature Schnauzers, Shetland Sheepdogs, and Beagles. Secondary hyperlipidemia is more common in dogs and results from endocrinopathies like hypothyroidism, diabetes, and hyperadrenocorticism. Other conditions associated with hyperlipidemia include pancreatitis, protein-losing nephropathy, cholestasis, obesity/ diet, and some drugs.
Why Treat Hyperlipidemia?
Many animals will present with no clinical signs, and increased lipid levels may be found incidentally on routine blood screening. Lack of clinical signs does not justify ignoring the abnormal values however may be an indication for rechecking prior to further investigation. Commonly animals will have waxing and waning courses of vomiting, diarrhea, and abdominal pain. Owners may report the resolution of clinical signs with fasting. Severe hypertriglyceridemia (> 1000 mg/dl) has been associated with pancreatitis, hepatic steatosis, glomerular disease, gall bladder mucoceles, lipemia retinalis, cutaneous xanthomas, peripheral nerve paralysis, behavior changes, and other neurologic signs. Seizures may be diagnosed as idiopathic epilepsy because of a lack of other clinical signs related to hyperlipidemia. However, the increased serum lipids should be suspected as a cause if present. Severe hypercholesterolemia (> 800 mg/ dl) may lead to atherosclerosis but is considered very rare in dogs. There has been no established correlation between the magnitude of the increase in serum lipids and the severity of the clinical signs.
Diagnosis of hyperlipidemia
Lipemia is a turbidity of a sample caused by an accumulation of lipoprotein particles. The largest particles ‒ chylomicrons ‒ have the greatest potential to cause turbidity in the sample. Therefore lipemia usually indicates hypertriglyceridemia. Pure hypercholesterolemia should not result in lipemia, as the LDL/HDL molecules are too small to reflect light. During your investigation for hypertriglyceridemia, be aware that centrifugation removes chylomicrons which will artifactually lower the triglyceride level.
Step one ensures that elevated cholesterol and/or triglycerides are repeatable by testing the patient after a 12-hour fast. If an animal is diagnosed with a specific underlying disease, treat the disease first and then initiate follow-up therapy if needed. As of note, cats are rarely diagnosed with significant hyperlipidemia; rare cases can be due to a lipoprotein lipase deficiency.
Treatment of Hyperlipidemia
- Diet: Low-fat. Dietary fat pet foods are listed as a percent metabolizable energy (ME), percent dry matter basis (DM), or present as-fed basis. Many follow fat labels on an ME basis. Success can be achieved with Royal Canin Low Fat (16.3% fat on an ME basis in the canned and 15.7% fat on an ME basis in the dry) or the Waltham Low Fat diet. Other low-fat diets: Royal Canin GI low-fat, Hills I/D low-fat (not the regular Hills I/D), or Purina EN GI low-fat diets. Alternatively, you could have a home-cooked lower-fat diet (as low as ~12% on an ME basis) formulated by a veterinary nutritionist. Most diet-directed treatment of hyperlipidemia takes a month or more to see an effect.
- Omega-3 fatty acids: Reduce serum cholesterol and triglyceride concentrations by decreasing the synthesis of VLDL and LDL. Recall that VLDL is important for TG transport; LDL for cholesterol transport. Dose: 10-220 mg/kg/ day.
- Fibrates: Bezafibrate, fenofibrate, gemfibrozil. The primary mechanism of action: increases lipolysis of T.G.-rich lipoproteins by lipoprotein lipase; increases hepatic fatty-acid uptake; decreases hepatic TG production; increases clearance of LDLs.
- Bezafibrateat a dose of 4-10 mg/ kg/ day normalizes both cholesterol and TG. As of 2018 not available in the US.
- Fenofibrate (TriCor) acts similarly to bezafibrate. Fenofibrate is available in the US as 54 mg tablets and is administered as 0.5 to 1 tablet per dog per day, usually during the evening meal
- Gemfibrozil: not as efficacious as the two fibrates above
- Chitin or Chitosan: For use in feline hyperlipidemia. Chitosan is a fiber supplement made from shellfish that reportedly binds lipids in diet and decreases absorption. No studies prove efficacy in dogs or cats.
- Niacin: Acts primarily to reduce hepatic triglyceride synthesis and VLDL production. Newer agents, e.g., Acipimox, also act to reduce adipose lipolysis. Niacin has vasodilatory effects and could cause some skin reddening. It might be reduced by giving it with meals or using a “no flush” niacin product or a slow-release product. Occasionally dogs seem uncomfortable and may scratch at their face afterward. Dose: 50-200mg/day/dog; dose can be divided into two daily doses. Some reports say Niacin is minimally effective.
- Statins/HMG CoA-reductase inhibitors (lovastatin, simvastatin, pravastatin, fluvastatin, cerivastatin, atorvastatin). Effective at reducing cholesterol levels by reducing hepatic cholesterol synthesis, thereby up-regulating LDL-receptor activity. They are the most powerful cholesterol-lowering agents available. Adverse effects: increased appetite, possible hepatotoxicity. Myopathy if combined with a fibrate. Dose: 2 mg/kg/day
- 5-Aminolevulinic Acid. Used for hypertriglyceridemia by increasing mitochondrial activity, thereby improving lipid metabolism. This has been used to normalize triglycerides in overweight Miniature Schnauzers.
Summary
Understanding lipid metabolism aids in understanding lipid profile abnormalities in dogs and cats. Although primary conditions have been reported, secondary hyperlipidemia is more common in small animals. Therefore a thorough search for an underlying cause should be performed if persistently increased cholesterol and/or triglyceride levels are documented. Medical therapy should treat the underlying cause and restrict dietary fat. Other treatments can be considered if conservative therapy is adequate. However, the potential for adverse effects should be discussed with owners prior to instituting these therapies.
References
- Von Zychlinski A, Williams M, McCormick S, Kleffmann T (June 2014). “Absolute quantification of apolipoproteins and associated proteins on human plasma lipoproteins.” Journal of Proteomics. 106: 181–90.
- Liu M, Doi T, Shen L, Woods SC, Seeley RJ, Zheng S, et al. (May 2001). “Intestinal satiety protein apolipoprotein AIV is synthesized and regulated in rat hypothalamus.” American Journal of Physiology. Regulatory, Integrative, and Comparative Physiology. 280 (5): R1382-7
- Ramasamy I (December 2014). “Recent advances in physiological lipoprotein metabolism.” Clinical Chemistry and Laboratory Medicine. 52 (12): 1695–727.
- Ooi EM, Barrett PH, Chan DC, Watts GF (May 2008). “Apolipoprotein C-III: understanding an emerging cardiovascular risk factor.” Clinical Science. 114(10): 611–24.
- Furrow E, Lees GE, Brown CA et al. Glomerular lesions and proteinuria in miniature schnauzer dogs. Vet Pathol 2017; 54: 484-89
- Kutsunai M, Kanemoto H, Fukushima K, et al. The association between gall bladder mucoceles and hyperlipidemia in dogs: a retrospective case-control study. Vet J 2014; 199: 76-79.
- De Marco V, Noronha KSM, Casado TC, et al. Therapy of canine hyperlipidemia with bezafibrate. J Vet Intern Med 2017; 31: 717-722.
- Bonaparte A, Tansey C, Wiebe M, et al. The effect of atorvastatin on haemostatic parameters in apparently healthy dogs. J Small Anim Pract 2019; 60:565-70.
- Parker V. Proceedings Advanced Endocrinology Nov 2-4 2021. Nutritional Management of Lipid Disorders- and How to interpret Pet food labels. 8-9.
- Xenoulis PG, Cammarata PJ, Walzem RL, et al. Serum triglyceride and cholesterol concentrations and lipoprotein profiles in dogs with naturally occurring pancreatitis and healthy control dogs. J Vet Intern Med 2020; 34: 644-652.
Plumb’s veterinary drug handbook, 9th edition. Wiley – Blackwell 2018.