-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Referrals
- Referral Forms/Contact
- Direct Connect
- Referring Veterinarian Portal
- Clinical Articles
- Partners in Care Newsletter
CE, Internships & Alumni Info
CE Seminar Schedule
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
By Martin Coster, DVM, MS, DACVO
www.angell.org/eyes
ophthalmology@angell.org
617-541-5095
Part One: Anatomy & Diagnosis
Anatomy of Lens Stability
The lens of the eye sits in the patellar fossa. Although you might have thought this structure to be found in the knee, it is actually the depression in the anterior face of the vitreous, that itself is formed by the posterior convexity of the lens. Anteriorly, the lens abuts the iris, which provides it a measure of support. Around the equator of the lens are the lens zonules (or Zonules of Zinn, which form the suspensory ligament of the lens). These zonules anchor the lens capsule to the ciliary body, which is responsible for accommodation or focusing of the lens.
Diagnosis of Lens Luxation
Lens luxation is the full dislocation of the lens out of the patellar fossa, either anteriorly (into the anterior chamber in front of the iris) or posteriorly (into the vitreous) (Curtis 1990). Both types of luxation can be surprisingly hard to diagnose, either due to very subtle changes or dramatic changes (e.g. corneal edema from glaucoma) that preclude full visualization of the lens.

Figure 2: Anterior lens luxation. Note the refractile edge of the lens from the 9 to 12 o’clock positions.
Anterior lens luxation with cataract is often very obvious (Figure 1), but when the lens is clear or when corneal edema from glaucoma is present, it can be hard to visualize. One feature to look for in this scenario is the positioning of the iris. Generally, the curvature of the iris (which is normally convex only because it lies over the convex lens surface) should be almost parallel with the curvature of the cornea. A slitbeam from a transilluminator can illuminate both structures well. If you see a concave surface to the iris (bending away from you centrally), this can imply the lens is in front of the iris, and at this point you should look peripherally around the limbus to attempt to visualize the edge of the lens, which should reflect light as a bright crescent (Figure 2).
If the iris is lying flat (“D-shaped” anterior chamber), the lens may be posteriorly luxated (Figure 3). The best way to visualize this is sometimes via retinal fundic examination, or in the event of visual axis impairment (eg from hyphema), ocular ultrasonography (Figure 4).

Figure 3: Posterior cataractous lens luxation. The retina is also degenerate resulting in marked tapetal hyperreflectivity.

Figure 4: Annotated ultrasound of an eye with posterior lens luxation. Direct visualization was impossible due to hyphema.
Diagnosis of Lens Subluxation
Lens subluxation is the partial detachment of the lens from the ciliary body, due to breakdown or weakness of the zonules. Although the presence of an “aphakic crescent” is the classic sign of lens subluxation (Figure 5), evidence of lens subluxation can be very subtle. Signs to look for can include an asymmetrically shallow anterior chamber (from one side of the lens tilting and pushing the iris forward), fluttering movement of the lens (phacodonesis) or iris (iridodonesis) as the eye moves (click here to view this in a human), and very commonly, liquefied vitreous in the anterior chamber. Subluxation can also be accompanied by an increase in intraocular pressure (IOP), ie secondary glaucoma. To confirm a diagnosis of lens subluxation when some of these symptoms are present, examination in a darkened room with a dim slitbeam from an ophthalmoscope can allow enough natural iris dilation to observe the subluxated edge of the lens, when looking across the eye at an angle.
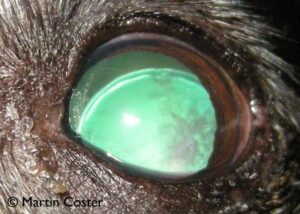
Figure 5: Lens subluxation. Note the aphakic crescent superiorly. The lens appears iridescent due to retro-illumination from the tapetal reflection. There is also a cataract, an opacity to retro-illuminated light at the righthand (lateral) aspect of the lens.
Even though it would help diagnosis, it bears emphasis that an eye with a suspected lens luxation or subluxation should never be iatrogenically dilated with tropicamide, atropine, or any other mydriatic drug. Dilating an eye with a subluxated lens removes the support of the iris from the lens’ anterior face, and can precipitate full luxation anteriorly. Dilating an eye with posterior luxation increases the risk that the lens will move forward in the eye. Additionally, pupil dilation can close the filtration angle, increasing IOP and potentially precipitating a glaucoma crisis.
That said, mydriatic agents are sometimes used by ophthalmologists in the management of lens luxation. Examples include: when pupillary block glaucoma is present (when the lens is anteriorly luxated and the pupil is constricted around vitreous, or when the pupil is tight against the lens like a closed ball valve); attempts to replace an anteriorly luxated lens with a procedure called “couching” (Montgomery, 2014); and in post-surgical (lensectomy) management (to reduce synechia formation, help with comfort, and stabilize the blood-ocular barrier).
Causes of Lens Instability
Lens luxation is known to be of genetic origin in many canine breeds (eg Terriers, Chinese Crested, American Eskimo, Australian Cattle Dog), likely autosomal recessive (Willis, Curtis et al. 1979; Farias, Johnson et al. 2010; Gould, Pettitt et al. 2011). DNA testing (for the ADAMTS17 substitution) is now available for these breeds from multiple sources: the Orthopedic Foundation for Animals, Optigen, and, in the UK, the Animal Health Trust. Otherwise, secondary lens luxation can occur from many conditions, including trauma, chronic glaucoma (buphthalmos, as stretching of the globe can tear the lens attachments), chronic uveitis, and hypermature cataracts.
In the cat, uveitis is the most common cause of lens luxation, which presumably occurs due to inflammatory breakdown of the lens’ suspensory ligament. Therefore, in cats an infectious disease workup (FeLV, FIV, FIP, toxoplasmosis, etc) is important when presented with a lens luxation (Olivero, Riis et al. 1991). Congenital anatomic defects have also been reported (Molleda, Martin et al. 1995).
Sequelae to Lens Instability
Lens instability can lead to uveitis, glaucoma (Curtis, Barnett et al. 1983), retinal detachment, hyphema, cataract, reduced vision, and blindness from sequelae. Uveitis likely occurs from lens motion stimulating inflammation of the iris, ciliary body, and even corneal endothelium in full anterior luxation. Glaucoma can occur as a sequel to uveitis (either acute or chronic build-up of inflammatory membranes or pre-iridal fibrovascular membranes that occlude the filtration angle). Glaucoma can also occur due to a primary obstruction of aqueous humor filtrate through the filtration angle. Dogs are generally at much higher risk of glaucoma than cats, due to their disparate ratios of lens to anterior chamber volumes, and a lens in the anterior chamber leaves little space for fluid to flow through the pupil out the angle. Additionally, anterior lens movement typically brings vitreous forward, which can become entrapped in the pupil. Retinal detachment can occur from the remaining lens zonular attachments at the peripheral retina exerting more pulling force on the retina as the lens begins to luxate. This, or direct irritation and inflammation of iris vasculature, can lead to hyphema. Cataract forms in the lens as the typically-nourishing aqueous humor alters in flow around the lens, reducing nutritional support to the lens. Reduced vision occurs from altered refraction / focussing of light onto the retina, or from any of the above sequelae, which can all of course lead to complete blindness.
Part Two: Medical & Surgical Management
Medical Management of Lens Instability
When diagnosed early, lens subluxation and its sequelae can be medically managed. Therapy is generally directed at preventing or treating glaucoma and uveitis. Glaucoma medications that reduce aqueous humor production (eg carbonic anhydrase inhibitors q8h [dorzolamide, brinzolamide] and beta blockers q12h [timolol]) are generally safe in most instances of lens instability. Dorzolamide does not affect pupil size (Plummer, MacKay et al. 2006), and although timolol can affect pupil size in both dogs and cats (Wilkie and Latimer 1991; Wilkie and Latimer 1991), in the present author’s experience this is a clinically insignificant effect. Negative effects of timolol on cardiac function (eg heart rate / bradycardia) should be considered and monitored for (Plummer, MacKay et al. 2006), especially in small patients.
Miotic agents such as latanoprost and demecarium bromide, in addition to providing excellent glaucoma control, have a special indication in lens instability. Pupillary constriction increases the lens-iris contact area, and can provide enhanced support to the lens, reducing the risk of a subluxated lens from fully luxating (Binder, Herring et al. 2007). In that report, vision was maintained for 1 year in 16 of 20 (80%) eyes and for 2 years in 11 of 19 (58%) of eyes. Miotic therapy delayed anterior lens luxation in eyes with lens instability.
Miosis will also help keep a posteriorly luxated lens in the posterior segment, reducing the potential for anterior movement. Prophylactic therapy of the second eye should also be considered, typically with a miotic agent q 12-24 h.
In the event of anterior lens luxation, a miotic agent may be contraindicated, as miosis can entrap the lens and attached vitreous humor and increase the risk of pupillary block glaucoma developing. I therefore educate clients to not give latanoprost if they see evidence of anterior luxation, and monitor these patients closely.
Uveitis must often be controlled in cases of lens instability. Movement of the lens can directly inflame the iris and choroid, and aqueous humor dynamics are altered by lens instability. For anti-inflammatory therapy, I prefer topical steroids (eg prednisolone acetate, dexamethasone in alcohol) over topical non-steroidal anti-inflammatory drugs (NSAID, eg flurbiprofen, diclofenac), due to potential exacerbation of glaucoma with topical NSAIDs. An oral NSAID (eg carprofen, meloxicam), can however be helpful for both inflammation and pain control, in dogs.
In non-glaucomatous anterior lens luxation (which is common in cats) the initial discomfort and inflammation can often be managed with topical anti-inflammatories and oral pain control (e.g. NSAID and tramadol in dogs, buprenorphine in cats), along with prophylactic therapy (e.g. dorzolamide q 8-12 h) to reduce the risk of glaucoma. Many pets will adapt, becoming apparently non-painful after a few weeks of therapy. As long as glaucoma does not occur and there are no symptoms of pain, anterior luxation can even be medically managed longterm (Figure 6). In these cases, however, elective lens removal surgery should be considered, due to the risk of glaucoma, lens-induced uveitis, and other sequelae such as retinal detachment. Earlier lens removal likely correlates greater with surgical and visual success (Stuhr, Schilke et al. 2009). When glaucoma or severe pain is present due to lens luxation, emergency surgical management is advocated.
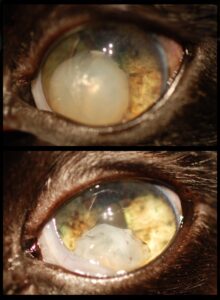
Figure 6: Anterior cataractous lens luxation in a cat, initial presentation and one year later. The cataract became hypermature (shrinking with a wrinkled lens capsule). In this cat, vision improved as the visual axis opened up. This result is atypical – this cat was treated longterm with anti-glaucoma and anti-inflammatory medications and monitored closely, and blinding or painful sequelae from the lens luxation fortunately did not occur.
Surgical Management of Lens Instability
Generally, lens subluxation is medically managed as above. However, when cataract is the cause of lens subluxation and vision is impaired, or when lens subluxation is progressing or causing uveitis, then lens extraction surgery should be considered. Extracapsular lens extraction refers to a surgery performed to remove the lens nucleus and cortex, leaving the lens capsule behind. Phacoemulsification cataract surgery is the most common example of this (see video). Depending on the severity of lens subluxation, surgery may be performed routinely, or may require the intraoperative insertion of a capsular tension ring, which provides 360 degree outward pressure from within the lens capsule, stabilizing the lens (see video).
“Couching” is the earliest known form of cataract surgery, described in people as early as 1700 BC, but still performed in various parts of the world (Omoti 2005). In this procedure, a sharp thorn or needle (inserted at the limbus) is used to push a cataractous lens into the vitreous, posteriorly luxating the lens. A recent report describes rolling a cotton swab along the cornea with heavy pressure, to push the lens posteriorly, without the need to introduce a needle into the eye (Montgomery, Labelle et al. 2014). Seventeen of 20 lenses were successfully posteriorly reduced, with only one recurrence (post-reduction topical latanoprost was used in all cases). Nine dogs remained blind after reduction; 6 of 11 eyes (54.5%) retained vision, and the median time to blindness (from glaucoma or retinal detachment) in the other 5 cases was 12 months.
Surgical removal of a luxated lens including the capsule is called intracapsular lens extraction (ICLE). In the “open sky” approach, the superior cornea is incised 120 to 180 degrees to remove the lens whole (see video). In an early study, 41 of 57 eyes (72%) had immediate post-operative vision, with this number declining to 61% at 3 months and 53% (8/15 eyes) at 12 months (Glover, Davidson et al. 1995).
The eye may be left aphakic (without a lens), or an intraocular lens (IOL) may be sutured to the sclera to sit in the posterior chamber (sulcus IOL, distinct from placement of IOLs in the lens capsule in routine phacoemulsification cataract surgery) (Nasisse, Glover et al. 1995; Wilkie, Gemensky-Metzler et al. 2008; Stuhr, Schilke et al. 2009). In the most recent report of sulcus IOL fixation, vision was maintained in 14 of 20 (70%) eyes with mean vision loss in the other 6 eyes occurring at 41 months (Stuhr, Schilke et al. 2009). Post-operative complications of lens removal can include hemorrhage, acute and chronic uveitis, corneal ulceration, glaucoma, retinal detachment or degeneration, and resultant blindness.
In conclusion, early diagnosis of lens instability with management of related disease processes is extremely important in the success of medical or surgical management. Examination and longterm follow-up by a veterinary ophthalmologist is recommended.
For more information about Angell’s Ophthalmology service, please visit www.angell.org/eyes. Dr. Coster can be reached for consults or referrals at 617-541-5095 or ophthalmology@angell.org
Surgical Videos:
Routine Phacoemulsification Cataract Surgery
Capsular Tension Ring Placement
Further Reading (Case Reports from the Canadian Veterinary Journal):
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3196025/
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3157063/
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3239160/
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC340155/
References:
Binder, D. R., I. P. Herring, et al. (2007). “Outcomes of nonsurgical management and efficacy of demecarium bromide treatment for primary lens instability in dogs: 34 cases (1990-2004).” J Am Vet Med Assoc 231(1): 89-93. [Pubmed]
Curtis, R. (1990). “Lens luxation in the dog and cat.” Vet Clin North Am Small Anim Pract 20(3): 755-73. [PubMed]
Curtis, R., K. C. Barnett, et al. (1983). “Clinical and pathological observations concerning the aetiology of primary lens luxation in the dog.” Vet Rec 112(11): 238-246. [PubMed]
Farias, F. H., G. S. Johnson, et al. (2010). “An ADAMTS17 splice donor site mutation in dogs with primary lens luxation.” Investigative Ophthalmology and Visual Science 51(9): 4716-21. [PubMed]
Glover, T. L., M. G. Davidson, et al. (1995). “The intracapsular extraction of displaced lenses in dogs: a retrospective study of 57 cases (1984-1990).” J Am Anim Hosp Assoc 31(1): 77-81. [Pubmed]
Gould, D., L. Pettitt, et al. (2011). “ADAMTS17 mutation associated with primary lens luxation is widespread among breeds.” Veterinary Ophthalmology 14(6): 378-84. [PubMed]
Molleda, J. M., E. Martin, et al. (1995). “Microphakia associated with lens luxation in the cat.” J Am Anim Hosp Assoc 31(3): 209-212. [Pubmed]
Montgomery, K. W., A. L. Labelle, et al. (2014). “Trans-corneal reduction of anterior lens luxation in dogs with lens instability: a retrospective study of 19 dogs (2010–2013).” Veterinary Ophthalmology 17(4): 275-279. [Pubmed]
Nasisse, M. P., T. L. Glover, et al. (1995). “Technique for the suture fixation of intraocular lenses in dogs.” Vet Comp Ophthalmol 5(3): 146-150.
Olivero, D. K., R. C. Riis, et al. (1991). “Feline lens displacement. A retrospective analysis of 345 cases.” Prog Vet Comp Ophthalmol 1(4): 239-244.
Omoti, A. E. (2005). “Complications of traditional couching in a Nigerian local population.” West African Journal of Medicine 24(1): 7-9. [Pubmed]
Plummer, C. E., E. O. MacKay, et al. (2006). “Comparison of the effects of topical administration of a fixed combination of dorzolamide-timolol to monotherapy with timolol or dorzolamide on IOP, pupil size, and heart rate in glaucomatous dogs.” Veterinary Ophthalmology 9(4): 245-249. [Pubmed]
Stuhr, C. M., H. K. Schilke, et al. (2009). “Intracapsular lensectomy and sulcus intraocular lens fixation in dogs with primary lens luxation or subluxation.” Veterinary Ophthalmology 12(6): 357-360. [Pubmed]
Wilkie, D. A., A. J. Gemensky-Metzler, et al. (2008). “A modified ab externo approach for suture fixation of an intraocular lens implant in the dog.” Veterinary Ophthalmology 11(1): 43-48. [Pubmed]
Wilkie, D. A. and C. A. Latimer (1991). “Effects of topical administration of timolol maleate on intraocular pressure and pupil size in cats.” Am J Vet Res 52(3): 436-440. [Pubmed]
Wilkie, D. A. and C. A. Latimer (1991). “Effects of topical administration of timolol maleate on intraocular pressure and pupil size in dogs.” Am J Vet Res 52(3): 432-435. [Pubmed]
Willis, M. B., R. Curtis, et al. (1979). “Genetic aspects of lens luxation in the Tibetan terrier.” Vet Rec 104(18): 409-412. [PubMed]

