-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Referrals
- Referral Forms/Contact
- Direct Connect
- Referring Veterinarian Portal
- Clinical Articles
- Partners in Care Newsletter
CE, Internships & Alumni Info
CE Seminar Schedule
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 By Catherine Sumner, DVM, DACVECC
By Catherine Sumner, DVM, DACVECC![]()
angell.org/emergency
emergency@angell.org
781-902-8400
January 2022
In 2012, the Reassessment Campaign on Veterinary Resuscitation (RECOVER) issued a seven-part series of special articles in the Journal of Veterinary Emergency and Critical Care (JVECC). This initiative evaluated the existing literature on cardiopulmonary resuscitation (CPR) in both human and veterinary medicine to develop evidence-based and clinically relevant guidelines for cardiopulmonary arrest (CPA) and CPR in small animal practice and identify areas for future research. Five main guidelines were identified: Preparedness and Prevention, Basic Life Support (BLS), Advanced Life Support (ALS), Monitoring, and Post-Cardiac Arrest Care.
(RECOVER) issued a seven-part series of special articles in the Journal of Veterinary Emergency and Critical Care (JVECC). This initiative evaluated the existing literature on cardiopulmonary resuscitation (CPR) in both human and veterinary medicine to develop evidence-based and clinically relevant guidelines for cardiopulmonary arrest (CPA) and CPR in small animal practice and identify areas for future research. Five main guidelines were identified: Preparedness and Prevention, Basic Life Support (BLS), Advanced Life Support (ALS), Monitoring, and Post-Cardiac Arrest Care.
The Preparedness and Prevention category includes guidelines about equipment organization, cognitive aids, training, and communication during CPR. One of the most critical steps that a clinic can take to be prepared for a CPA event is to have a crash cart or tackle box filled with all required supplies for CPR, including drugs and syringes for administration, intubation/ventilation supplies, surgical equipment, and any other necessities. This equipment should be well organized, checked routinely to ensure that all necessary supplies are present, and sealed to prevent cart usage at other times. Staff should be familiar with the locations of supplies within the crash cart. It is advisable to have a separate crash cart or tackle box (or bring one with the patient) in each area where patients are undergoing anesthesia. If possible, having a multi-parameter monitor, anesthesia machine, and defibrillator located in the same area as the crash cart is ideal, in addition to having access to IV fluids, IV catheter supplies, etc. Displaying cognitive aids such as drug dosing charts, algorithms, and flow charts is recommended. Staff members should receive didactic and hands-on CPR education; training should be repeated every six months to maintain knowledge and skills. As part of training, it has been found that having an evaluation after training results in more effective training, and it is also advised to have debriefing sessions with the entire team after any CPR attempt or mock CPR scenario. Having a leader (veterinarian or technician) during CPR can make an effort more organized, as this person can distribute tasks, ensure closed-loop communication, evaluate the quality of the CPR being performed, and consider the global status of the code. Having a pre-determined resuscitation code for every patient staying in the hospital or undergoing anesthesia is also a best practice.
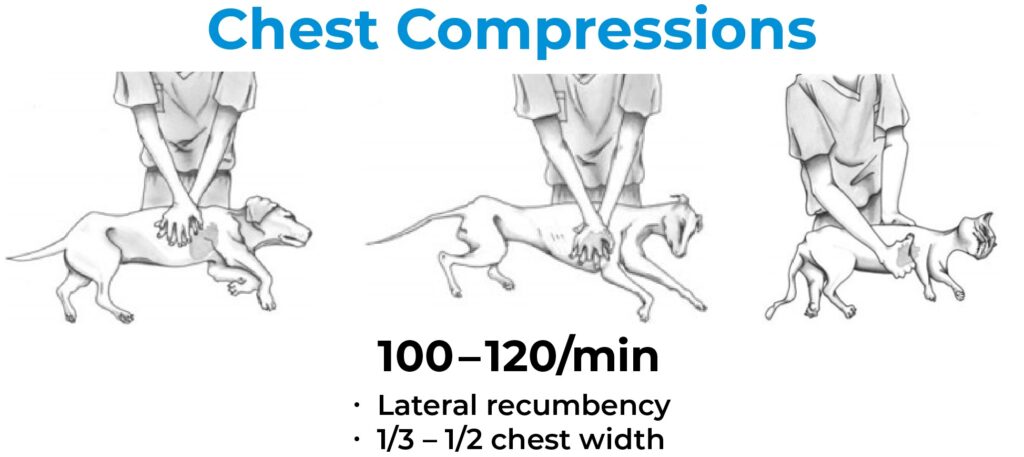
The Basic Life Support (BLS) category encompasses recognition of CPA, chest compressions, airway management, and ventilation. Importantly, the speed with which CPR is initiated and the quality of BLS performed is associated with the patient’s return of spontaneous circulation (ROSC) and ultimately survival from the CPA event. CPR should be commenced immediately if there is any concern for a CPA event. A quick Airway/Breathing/Circulation (ABC) check should be performed in an unresponsive patient, taking 5-10 seconds. Pulse palpation alone should not be relied on, as it has poor sensitivity. Chest compressions should be initiated at a rate of 100-120 compressions/minute, with a compression depth of 1/3-1/2 of the chest wall width, allowing for full chest wall recoil between each compression. Compressions should be performed in lateral recumbency in most patients, though there are some breed/conformation/size-specific variations. Intubation of the patient should be performed whenever possible and as soon as feasible. It is recommended to intubate the patient while receiving chest compressions to avoid a pause in compressions. Lateral intubation can be practiced regularly on routine anesthesia cases so that staff members are comfortable with this technique. Once intubated, ventilation should be provided at a rate of 10 breaths per minute, a tidal volume of 10 mL/kg, and an inspiratory time of one second. Chest compressions and ventilation should occur concurrently, with chest compressions delivered without interruption for two-minute cycles. It is advised to rotate the staff member performing chest compressions every two minutes to avoid fatigue and deterioration in the quality of compressions. The pause between two-minute cycles should be minimized as much as possible.
The Advanced Life Support (ALS) category includes other aspects of CPR such as drug therapy (vasopressors, positive inotropes, anticholinergics, reversal agents), defibrillation, correction of electrolyte, and acid-base changes, and fluid therapy. It is recommended to administer low-dose IV epinephrine during every other two-minute cycle of BLS, and in cases of prolonged CPR, high dose epinephrine can be considered. Vasopressin can be administered IV in the alternating BLS cycles to epinephrine. If IV or intraosseous access for administration is not available, epinephrine and vasopressin can be diluted with saline and administered via an intratracheal route, through a catheter longer than the endotracheal tube. Reversal agents (atipamezole, flumazenil, naloxone) can be administered if a reversible drug had been previously administered or overdose/toxicity is suspected. Defibrillation should be performed when an appropriate rhythm is detected (ventricular fibrillation, pulseless ventricular tachycardia), and a biphasic defibrillator is preferred to a monophasic. The timing of defibrillation will depend on how long ago CPA occurred. One shock should be administered, and then another cycle of compressions/ventilation should be initiated. Increasing the defibrillation dose by 50% with subsequent shocks can be considered. Treatment for documented hypocalcemia, hyperkalemia, or hypokalemia can be performed. Administration of corticosteroids is not recommended. IV fluids should be administered to patients suspected to be hypovolemic but not those that are euvolemic or hypervolemic. Supplemental oxygen can increase the FiO2, but ventilation with room air is also acceptable. In patients with intrathoracic disease such as pericardial effusion or tension pneumothorax, open chest CPR can be considered but requires a skilled team, extensive resources, and advanced supportive care; if ROSC is achieved, refer to a 24-hour facility for continued care.
The Monitoring category addresses methods to confirm CPA and monitoring during CPR, patients at risk for CPA, and patients post-ROSC. When diagnosing CPA, pulse palpation is unreliable, the time necessary to set up a Doppler is too long, and ECG rhythms can be misinterpreted as perfusing rhythms. Endotracheal intubation can be confirmed using an end-tidal CO2 (ETCO2) monitor, in conjunction with direct visualization and confirmation of chest excursions with administered breaths. During CPR, ETCO2 can be used to evaluate the efficacy of CPR, with higher ETCO2 associated with increased ROSC. An ECG evaluation during pauses between CPR cycles is recommended during CPR. The use of a Doppler can be problematic due to motion artifact due to compressions but can be evaluated during intercycle pauses. EtCO2, continuous Doppler, and continuous ECG monitoring are recommended in patients at risk for CPA. Similarly, in patients that have ROSC, aggressive monitoring is warranted to evaluate for recurrence of CPA.
The Post-Cardiac Arrest Care category is beyond the scope of this overview, as ideally, a patient that achieves ROSC would be transferred to a 24-hour facility for ongoing care.
Historically, the lack of standardized guidelines in veterinary medicine has led to signification variations in how CPR has been performed. With the release of the RECOVER guidelines, a study published in 2020 found that current CPR techniques have shifted to those recommended. A RECOVER 2.0 initiative is currently underway, which will add further information to that now available.