-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Referrals
- Referral Forms/Contact
- Direct Connect
- Referring Veterinarian Portal
- Clinical Articles
- Partners in Care Newsletter
CE, Internships & Alumni Info
CE Seminar Schedule
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 By Jennifer Peterson-Levitt, DVM, DACVS-SA
By Jennifer Peterson-Levitt, DVM, DACVS-SA![]()
angell.org/surgery
surgery@angell.org
617-541-5048
x
April 2023
x
x
Indications for Performing a Perineal Urethrostomy
A “urethrostomy” refers to creating a new, permanent opening in the urethra. The perineal area is the most common location chosen for urethrostomy in cats because it allows for urination from a normal anatomic region and facilitates the creation of a comparatively larger stoma in relation to the diameter of the natural urethral orifice. Alternative urethrostomy locations include (modified1) pre-pubic, subpubic, and transpelvic locations; however, these procedures are reserved for urethral lesions located cranial to the bulbourethral glands. All feline urethrostomies are performed at, or cranial to, the level of the bulbourethral glands because the feline urethra gradually tapers in diameter in a cranial to caudal direction with an average internal diameter of 2 mm at the pre- and immediate post-prostatic urethra, 1.3 mm at the level of the bulbourethral glands, and 0.7 mm at the terminal portion of the urethra.2 A perineal urethrostomy is most commonly performed as a component of management for Feline Lower Urinary Tract Disease (FLUTD) but can also be utilized to treat distal urethral trauma, stricture, neoplasia, or congenital anomalies. Cats with FLUTD are considered candidates for a perineal urethrostomy when other urethral obstruction causes have been ruled out, and cats have continued to develop recurrent urethral obstructions despite appropriate medical management.
Procedure Description

Figure 1
Perineal urethrostomies can be performed in both dorsal and sternal recumbency. Regardless of the positioning, the patient is placed with the head towards the anesthesia machine and the perineal area at the opposite end of the table to minimize the table distance between the patient and surgeon. An anal purse-string suture should be placed to minimize intra-operative fecal contamination. Patients positioned in dorsal recumbency should have their legs gently positioned cranially and laterally to expose the perineal area (Figure 1) maximally. Patients in sternal recumbency are positioned with the pelvic limbs hanging off the end of the table and the tail gently positioned over the dorsum to maximize exposure (Figure 22). Additional padding can be placed under the lumbar area (when in dorsal recumbency) or the caudoventral abdomen (when in sternal recumbency) to support the patient and further elevate the perineal area.
Although dorsal recumbency has been advocated in patients requiring a concurrent cystotomy to avoid

Figure 2
the need for repositioning between procedures, there is no significant difference in complication rates or the duration of surgery or anesthesia between positions.3 A decreased briskness of the perineal reflex and an increased occurrence of spinal pain have been seen in patients 24 hours following surgery; however, there was no difference in the rate of occurrence between patients positioned in dorsal or sternal recumbency.4
The perineal area is fully clipped and aseptically prepped for surgery. If a cystotomy is planned under the same anesthesia, the patient can be positioned in dorsal recumbency, and the ventral abdomen can be prepped and draped into the same operating field to avoid the need for repositioning between procedures. If possible, a urethral catheter should be placed before initiating surgery to help facilitate identification and dissection. A blade creates an elliptical incision around the scrotum and prepuce. Intact males are routinely neutered. The distal tip of the penis and/or prepuce can be grasped and manipulated with Allis tissue forceps to ease dissection. The penis is isolated and circumferentially dissected to the level of insertion of the ischiocavernosus muscles on the penis using a combination of sharp and blunt dissection. Monopolar and/or bipolar electrosurgery can help minimize bleeding during dissection (Figure 3). The bilateral ischiocavernosus muscles are

Figure 3
completely elevated from their origin on the ischium. Electrocautery or a blade can initiate the elevation, which is completed using a freer periosteal elevator to minimize the risk of hemorrhage from the muscle. Releasing the ischiocavernosus muscles allows exposure of the ventral penile ligament, which is sharply transected at the insertion on the ventral and central portion of the penis. Circumferential dissection of the penis from the subcutaneous tissue is continued, and the retractor penis muscle is sharply transected from the dorsal aspect of the penis (Figure 4). Circumferential dissection is continued until the surgeon has exposed the bulbourethral glands. These are best seen and palpated on the dorsal aspect of the penis and are located just cranial to the transected ischiocavernosus muscles.
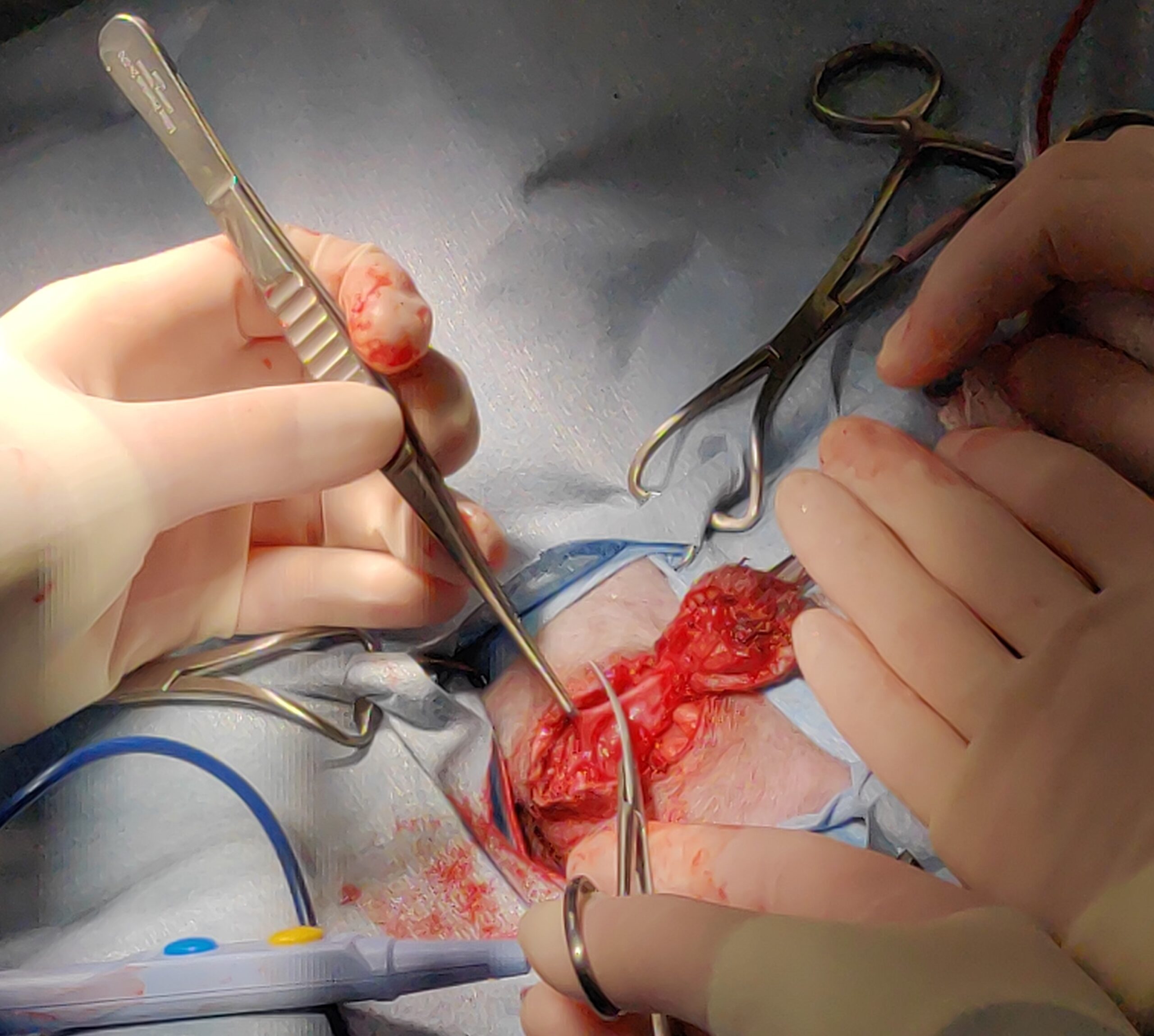
Figure 4
Once the penis has been adequately dissected, a blade or fine tenotomy scissors are used to incise the penile urethra from its distal tip cranially to the level of the bulbourethral glands. Failure to incise the urethra far enough cranially limits the size of the urethrostomy site and increases the risk for stricture formation. If a urethral catheter cannot be placed pre-operatively due to obstruction, a catheter should be placed following the urethral incision to help guide the creation of an appropriate urethrostomy. The post-operative urethrostomy luminal diameter has been shown to decrease by an average of 0.15±0.09 mm2 by 12 days post-operatively, so the urethrostomy site should be large enough to tolerate this anticipated stricturing that occurs as a natural part of healing.5 A stoma that can easily accommodate a 10Fr red rubber catheter at the time of surgery has a 6% chance of developing an obstructive stricture, while stomas that can maximally accept an 8Fr or 6Fr catheter have a 44% and 100% chance of developing obstructive strictures respectively.5
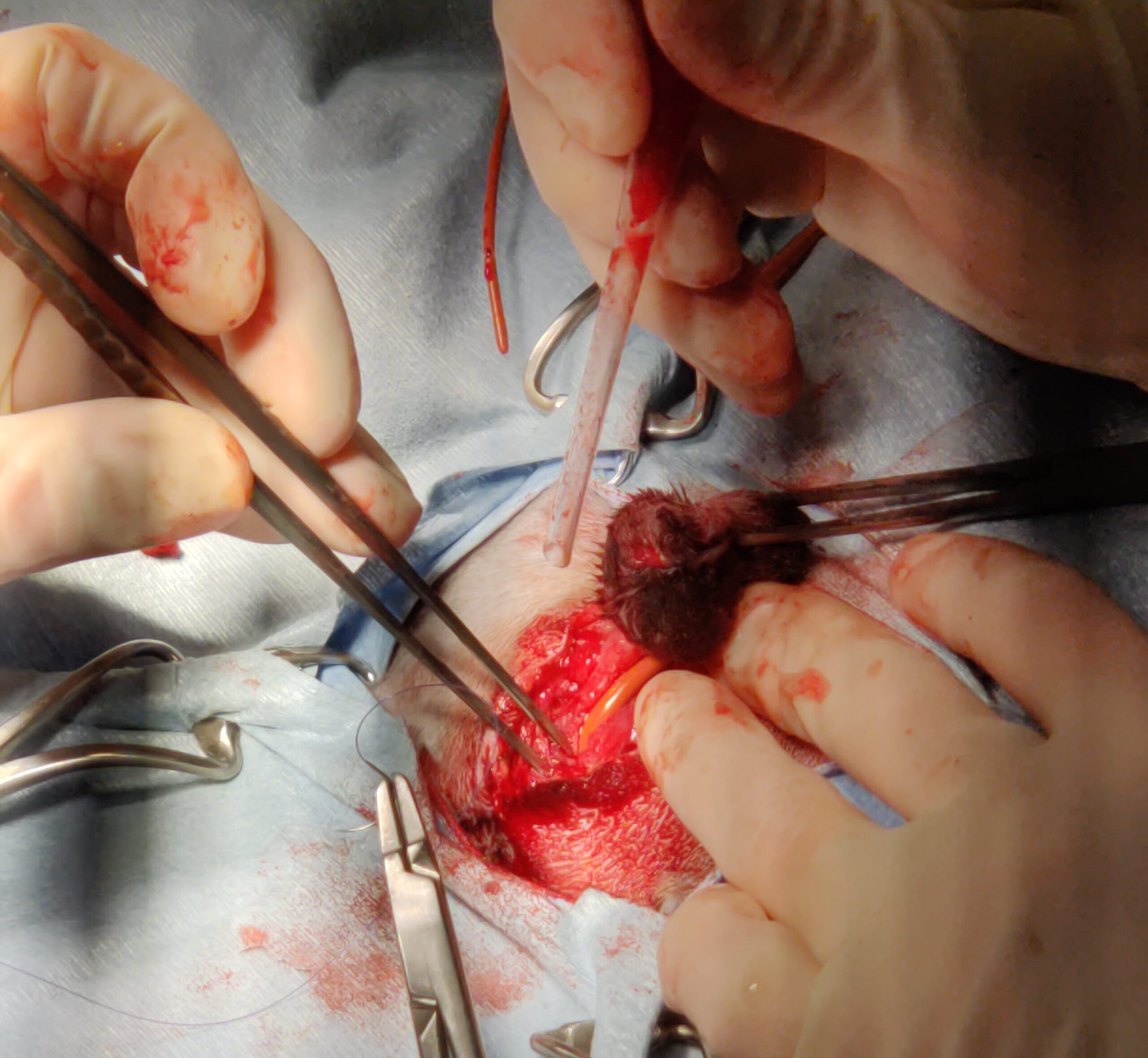
Figure 5
The urethrostomy is formed by suturing the urethral mucosa to the surrounding skin. Any tension on the site should be avoided to minimize the risk of dehiscence and excessive stricturing of the site. While non-absorbable (ex.: Nylon) and slowly absorbable (ex.: polydioxanone) sutures can be used, rapidly absorbable sutures (ex.: poliglecaprone 25) have been shown to be safe and eliminate the need for suture removal.6 A simple interrupted or horizontal mattress suture is placed at the dorsal extent, or 12 o’clock position, of the urethrostomy site to maintain appropriate orientation and avoid malpositioning of the urethra. Simple interrupted sutures are placed on either side of the urethrostomy to gradually create the opening and avoid tension between the two sides. A 10Fr urethral catheter can be left in place during the creation of the stoma to ensure adequate size (Figure 5). Alternately, based on surgeon preference, the catheter can be placed intermittently during the creation of the stoma to confirm the appropriate diameter. A “washboard” can be created using an approximately 1cm long segment of the remaining penile urethra. This 1cm strip of penile mucosa is sutured to the surrounding skin using either simple interrupted or simple continuous sutures. It serves to minimize tension on the site and minimize urine scald. Any penile tissue that remains following the creation of the “washboard” is ligated with a circumferential or transfixing ligature and then amputated. Final sutures are placed in either corner of the distal extent of the “washboard,” the remainder of the skin is routinely closed using a two-layer closure (subcutaneous tissue and skin).
Outcome
Although good to excellent outcomes have been reported long-term in 81.8 to 100% of cases, it is important to remember that a perineal urethrostomy is a salvage procedure.7,8 Owners should understand that a perineal urethrostomy can be used to manage FLUTD but is not a cure for the disease. Approximately 54% of cats develop short-term complications, and urinary obstruction and urethrostomy site stricture have been reported in up to 20% of patients at an average of 92±25 days post-operatively. 5,9 Sterile cystitis and urinary tract infections are the most common short- and long-term complications; however, other less common short-term complications reported include urinary incontinence, recurrent obstructions, strictures, urine extravasation into the perineal subcutaneous tissues, and regional dermatitis.9 Minor long-term complications are less common; however, 13.5% to 39% of patients report recurrent bouts of sterile cystitis and/or urinary tract infections consistent with FLUTD.6,9 Although subclinical in some patients, bacteriuria was seen in 77.2% of all cats 12 to 24 months following a perineal urethrostomy.8
In summary, perineal urethrostomies are commonly performed procedures utilized as a component of FLUTD management in cats. Although the procedure is associated with a fairly high rate of short-term complications, it has a high long-term success rate. It has been consistently shown to improve the quality of life in affected cats.7,8
x
References
- L Bresciani. Modified pre-pubic urethrostomy with body wall tunneling: Description oftechnique and long-term outcome in eight male cats. Vet Surg. 2022;51:353-360
- SA Johnston and KM Tobias. Veterinary Surgery Small Animal. Elsevier. St. Louis, Missouri. 2nd Edition. 2018;117:2234-2246.
- AK Nye, JK Luther, FA Mann, K Thieman Mankin, H Phillips, KJ Goode, P Schwartz, NT Squire, JJ Runge, EA Swanson, DR Dugat. Retrospective multicentric study comparing durations of surgery and anesthesia and likelihoods of short- and long-term complication between cats positioned in sternal or dorsal recumbency for perineal urethrostomy. JAVMA. 2020; 257(2):176-182.
- P Slunsky, M Brunnberg, S Loderstedt, A Haake, L Brunnberg. Effect of intraoperative positioning on post-operative neurological status in cats after perineal urethrostomy. JFMS. 2019:21(10)931-937.
- U Segal, J Shani, O Zemer, R Joseph. Evaluation of urethral orifice cross-section dimension following perineal urethrostomy in male cats. JSAP. 2020;61:475-479
- DL Frem, HA Hottinger, SL Hunter, NJ Trout. Use of poliglecaprone 25 for perineal urethrostomy in cats: 61 cases (2007-2013). JAVMA. 251(8):935-940.
- MR Slater, S Pailler, JM Gayle, I Cohen, EL Galloway, KA Frank, C DeClementi. Welfare of cats 5-29 months after perineal urethrostomy: 74 cases (2015-2017). JFMS. 20202;22(6):582-588.
- RP Sousa-Filho, DCS Nunes-Pinheiro, KO Sampaio, ECB da Silva, GASA Cavalcanti, MGMC Mori da Cunha. Clinical outcomes of 28 cats 12-24 months after urethrostomy. JFMS. 2020:22(10):890-897.
- M Seneviratne, P Stamenova, K Lee. Comparison of surgical indications and short- and long-term complications in 56 cats undergoing perineal, transpelvic, or pre-pubic urethrostomy. JFMA. 20201:23(6):477-486.