-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Referrals
- Referral Forms/Contact
- Direct Connect
- Referring Veterinarian Portal
- Clinical Articles
- Partners in Care Newsletter
CE, Internships & Alumni Info
CE Seminar Schedule
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 By Evan Mariotti, DVM, DACVIM (SAIM)
By Evan Mariotti, DVM, DACVIM (SAIM)![]()
angell.org/internalmedicine
internalmedicine@angell.org
617-541-5186
April 2022
Anatomy and Physiology of the Thyroid Gland
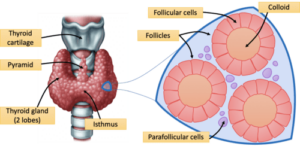
In humans, the thyroid gland is located ventral to the trachea, with both lobes connected by an isthmus. In cats, there is no isthmus, and thus both lobes are separated and located on both sides of the trachea. It is made of glandular tissue with cells in follicles. Follicles are filled with colloid that incorporates the main storage of thyroid hormones. There are also parafollicular cells outside of the follicles that secrete calcitonin.
The synthesis of thyroid hormones occurs within the thyroid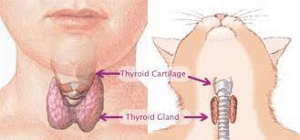 follicular cells and the colloid. Iodine is taken into the body and converted to iodide in the gastrointestinal tract. It is transported into the follicle cells by the Na+/I- symporter, oxidized in the follicular cell to the active form, and then moves into the colloid. A molecule called thyroglobulin is synthesized and undergoes exocytosis into the colloid. The thyroglobulin is then iodinized by thyroid peroxidase into monoiodotyrosine (MIT) and diiodotyrosine (DIT). MIT and DIT are either linked together to form T3 or DIT links with another DIT to form T4. Thyroglobulin then undergoes endocytosis into the follicular cells then fuses with a lysosome that cleaves off T3 and T4 via hydrolysis. T3 and T4 then leave the thyroid follicular cells to peripheral tissues. In those tissues, T4 is converted to the active form of T3.
follicular cells and the colloid. Iodine is taken into the body and converted to iodide in the gastrointestinal tract. It is transported into the follicle cells by the Na+/I- symporter, oxidized in the follicular cell to the active form, and then moves into the colloid. A molecule called thyroglobulin is synthesized and undergoes exocytosis into the colloid. The thyroglobulin is then iodinized by thyroid peroxidase into monoiodotyrosine (MIT) and diiodotyrosine (DIT). MIT and DIT are either linked together to form T3 or DIT links with another DIT to form T4. Thyroglobulin then undergoes endocytosis into the follicular cells then fuses with a lysosome that cleaves off T3 and T4 via hydrolysis. T3 and T4 then leave the thyroid follicular cells to peripheral tissues. In those tissues, T4 is converted to the active form of T3.
 Thyroid hormone penetrates the cell membranes and acts on the nucleus to initiate mRNA transcription. This leads to increases in oxygen consumption, increases in heat production, enhancement of the sympathetic nervous system effects by beta-adrenergic receptors, increases in heart rate and contractility, and increased lipolysis, among several other actions. Thyroid hormone is essential for normal growth. Without it during development, animals are born and disproportionate dwarf or they die in utero.
Thyroid hormone penetrates the cell membranes and acts on the nucleus to initiate mRNA transcription. This leads to increases in oxygen consumption, increases in heat production, enhancement of the sympathetic nervous system effects by beta-adrenergic receptors, increases in heart rate and contractility, and increased lipolysis, among several other actions. Thyroid hormone is essential for normal growth. Without it during development, animals are born and disproportionate dwarf or they die in utero.
Feline Hyperthyroidism
Feline hyperthyroidism (FHT) is the most common endocrine disease in the cat. It has a 6% incidence rate in all cats over the age of 9-years-old, and that incidence rate is increasing. There is a thought that, potentially, this has to do with an increase in goitrogens in commercial cat food with varying degree of iodine as well. Hyperthyroid cats will most likely have bilateral adenomas with a greater than 50% chance of being asymmetrical. Unilateral disease occurs in much fewer patients. Cats can also have ectopic thyroid tissue anywhere from the thyroid gland area to the base of the heart. Thyroid carcinoma in cats is very rare.
disease in the cat. It has a 6% incidence rate in all cats over the age of 9-years-old, and that incidence rate is increasing. There is a thought that, potentially, this has to do with an increase in goitrogens in commercial cat food with varying degree of iodine as well. Hyperthyroid cats will most likely have bilateral adenomas with a greater than 50% chance of being asymmetrical. Unilateral disease occurs in much fewer patients. Cats can also have ectopic thyroid tissue anywhere from the thyroid gland area to the base of the heart. Thyroid carcinoma in cats is very rare.
Signs of FHT are commonly weight loss, goiter, a thin BCS, and heart murmur. Common diagnostics to detect FHT are total T4 and free T4. Less common diagnostics include the T3 suppression test, TRH stimulation test, and thyroid scintigraphy. Treatments for FHT include antithyroid drugs, limited iodine foods, radioactive iodine, and thyroidectomy, with each treatment having its own set of advantages and disadvantages.
Radioiodine Therapy
In the body, thyroid hormone and thyroglobulin are the only molecules that require iodine. Therefore, all ingested iodine goes only to the thyroid gland through the Na+/I- symporter. If iodine is tagged with radioactivity (I-131), beta particles will destroy the local tissues in the hyperactive adenomas. Adjacent normal tissues can also be destroyed by collateral damage. Radioiodine can be administered subcutaneously, intramuscularly, or through the mouth.
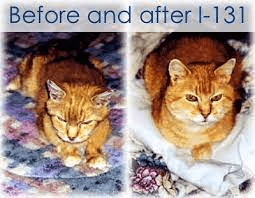 I-131 is indicated for cats with Methimazole reactions, owners who can’t medicate their cats, and owners looking for a cure. It is also considered for cats that don’t like the limited iodine diets and owners who want to avoid thyroidectomy. Diagnostics needed before therapy include full labs with three months of presentation (ideally a set of labs on and off of Methimazole), imaging of the chest and abdomen, and thyroid scintigraphy. As much as possible can be done at the local vet. After the appropriate diagnostics are performed, a dose of I-131 is carefully formed based on the results and patient condition. Some other facilities that perform radioiodine therapy may give the same dose to each patient (usually 3mCi). Angell uses 3mCi as a starting point, and increases or decreases may be made based on the diagnostics results.
I-131 is indicated for cats with Methimazole reactions, owners who can’t medicate their cats, and owners looking for a cure. It is also considered for cats that don’t like the limited iodine diets and owners who want to avoid thyroidectomy. Diagnostics needed before therapy include full labs with three months of presentation (ideally a set of labs on and off of Methimazole), imaging of the chest and abdomen, and thyroid scintigraphy. As much as possible can be done at the local vet. After the appropriate diagnostics are performed, a dose of I-131 is carefully formed based on the results and patient condition. Some other facilities that perform radioiodine therapy may give the same dose to each patient (usually 3mCi). Angell uses 3mCi as a starting point, and increases or decreases may be made based on the diagnostics results.
After treatment, we house the cats in a particular ward where we monitor them for any side effects of the treatment (anorexia, laryngitis, dehydration, etc.) and give any appropriate treatments. We keep the cats for a minimum of 72 hours post-treatment per Massachusetts state law. It is at the owner’s discretion if they want to take the cat home on all restrictions (contact and litter) or to board them for the full restriction timetable of 17 days after treatment when contact restrictions are lifted. Litter restriction can be lifted after 10 to 14 days.
A T4 and check of kidney values should be rechecked in one month and three months post-administration. If the patient is hypothyroid at the three-month mark, they will likely need supplementation with L-thyroxine. If the patient is persistently hyperthyroid, they can pursue any of the previous treatment options illustrated, but most commonly, they are retreated with radioiodine and will be euthyroid post-procedure in most cases.