-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Referrals
- Referral Forms/Contact
- Direct Connect
- Referring Veterinarian Portal
- Clinical Articles
- Partners in Care Newsletter
CE, Internships & Alumni Info
CE Seminar Schedule
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 By Daniel Biros, DVM ,DACVO
By Daniel Biros, DVM ,DACVO![]()
angell.org/eyes
ophthalmology@angell.org
617-541-5095
March 2022
Endophthalmitis
Blindness in cats can stem from a single ocular change such as a cataract to a more complicated systemic disease affecting multiple parts of the visual axis. Working through a relatively long list of differentials can be daunting. Gaining more familiarity with the diseases and abnormalities affecting the clarity and function of the feline visual axis will be our primary goal. With a thorough physical examination, a methodical eye evaluation, and a good history from the client, you can get an excellent idea of what pathological processes are going on and what treatment options, if any, are possible.
Asking the right questions
It is good to briefly review the tools and tests that will help diagnose the basic workup. For blindness, particularly, tonometry, direct or indirect ophthalmoscopy and a diffuse, bright illumination source such as a Finoff transilluminator (left) will provide the essential tools for an eye examination. Testing the visual reflex pathways is usually where most evaluations will start. The menace reflex, dazzle response, and pupillary light reflexes are integral to any eye examination, especially with reported vision loss. Ancillary ophthalmic testing such as fluorescein staining and Schirmer tear testing is less critical in the workup for blindness unless the cornea is involved. If the visual axis cannot be fully visualized, then ocular ultrasound may be helpful to characterize the ocular structures. When tissue changes are destructive or proliferative and do not respond to symptomatic treatment, cytology, bacterial culture, and even histopathology can be helpful if the tissue in question is readily accessible. When the lesions are deep or inaccessible and infectious disease is suspected, serology can assist, especially in posterior segment disease. Ocular toxoplasmosis and fungal diseases are often diagnosed with serology, among other systemic infections.
Having the right diagnostic tools

Finoff transilluminator
It is good to briefly review the tools and tests that will help diagnose the basic workup. For blindness, particularly, tonometry, direct or indirect ophthalmoscopy and a diffuse, bright illumination source such as a Finoff transilluminator (left) will provide the essential tools for an eye examination. Testing the visual reflex pathways is usually where most evaluations will start. The menace reflex, dazzle response, and pupillary light reflexes are integral to any eye examination, especially with reported vision loss. Ancillary ophthalmic testing such as fluorescein staining and Schirmer tear testing is less critical in the workup for blindness unless the cornea is involved. If the visual axis cannot be fully visualized, then ocular ultrasound may be helpful to characterize the ocular structures. When tissue changes are destructive or proliferative and do not respond to symptomatic treatment, cytology, bacterial culture, and even histopathology can be helpful if the tissue in question is readily accessible. When the lesions are deep or inaccessible and infectious disease is suspected, serology can assist, especially in posterior segment disease. Ocular toxoplasmosis and fungal diseases are often diagnosed with serology, among other systemic infections.
Ocular surface causes

Neonatal ophthalmia
Infections on the ocular surface can trigger significant eyelid and ocular surface changes at a young age, including eyelid fusion and conjunctival proliferation over the cornea, excessive corneal neovascularization, scarring, and at worst, deep corneal ulceration and perforation. Neonatal ophthalmia (right), ocular herpes keratitis, and conjunctivitis are the leading causes for changes like these. Ocular herpes can happen at any age with more severe, cyclic, or relentless cases of inflammation taking a toll on the corneal clarity and comfort. In cats, chronic ulceration (from ocular herpes or other causes) can also lead to corneal necrosis or sequestrum formation, where brown plaques develop in the ulcer bed of nonhealing ulceration. Brachycephalic cats are overrepresented. If untreated, these affected corneas can become obscured entirely with or without a neovascularization response. In severe or known progressive cases, surgical excision via lamellar keratectomy can restore some vision. Eosinophilic keratitis is another manifestation of chronic corneal and conjunctival inflammation unique to cats and, if untreated, can spread over the entire cornea, causing vision loss. Immunomodulatory therapy can be implemented topically to control the inflammation, but treatment is often long-term, if not life-long, to prevent relapses. Extensive corneal trauma, nonulcerative chronic keratitis (idiopathic), and diffuse corneal edema attributed conditions ranging from acute bullous keratopathy or congenital mucopolysaccharidosis can lead to permanent vision loss. However, cats can recover vision from acute bullous keratopathy with a supportive and specific treatment, including ophthalmic hypertonic saline preparations, third eyelid flaps, or conjunctival grafting (Gunderson type).
Anterior segment causes
Anterior Segment – Cataract
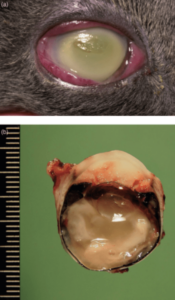
Cataract and glaucoma are the leading anterior segment causes for blindness in cats. Feline cataracts can be primary or hereditary, but a more common cause is cataract progression related to chronic uveitis. Because most cataract cases in cats are intrinsically linked to chronic uveitis and the real potential for secondary glaucoma, cataract surgery is far less often done in cats than dogs. The causes of uveitis are linked to idiopathic causes despite the usual workup of the identifiable differentials, including toxoplasmosis, fungal disease, lymphoma, and trauma. Uveitis per se does not cause vision loss unless a substantial amount of hyphema, hypopyon, or fibrin fills the anterior chamber, replacing the clear aqueous humor. Symptomatic medical treatment for the inflammation or identifying and addressing the nature of the bleeding quickly and aggressively is the best way to tackle loss of anterior chamber clarity. Ocular sepsis with bacteria due to trauma or a penetrating foreign body.
Other changes in the anterior segment that can cause blindness are expansive tumors within the eye, including neoplasia (adenomas, sarcomas, or nodular melanomas), lens luxation, and miosis in conjunction with scarring/adhesions. These conditions in advanced stages can obliterate the visual axis or trigger other secondary problems in vision, including retinal detachment, glaucoma, or corneal edema.
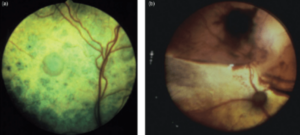
Posterior segment causes
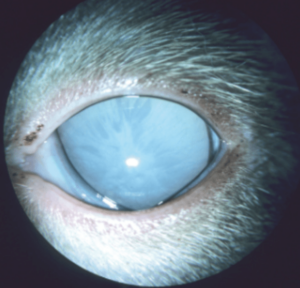
Hypertensive retinopathy
The most common presentation in our practice for sudden blindness in cats is hypertensive retinopathy (right). The retinas will detach and often bleed due to undiagnosed high blood pressure. Varying degrees of hyphema may also be seen if there is a tear to a retinal blood vessel as part of the presentation. These patients tend to be older and have coexisting heart or kidney disease. Managing systemic blood pressure is the best course of treatment for these patients and addressing any other associated systemic conditions.
The second most common posterior segment cause of blindness we see is diffuse retinal degeneration, which can result from chronic glaucoma, hereditary rod-cone photoreceptor disease, or in some cats, associated as a toxic effect of systemic enrofloxacin. There is no treatment for retinal degeneration in these cases. Other less severe forms of retinal degeneration typically do not cause complete blindness (e.g., taurine deficiency retinopathy). Even with extensive retinal degeneration, pupillary light reflexes in cats often remain intact, a unique feature of feline retinal degeneration.
Finally, infiltrative retinopathies may include infectious diseases such as toxoplasmosis, cryptococcosis, and tick-borne disease. Ocular changes resulting in retinal detachments, cellular granulomatous intraretinal plaques, and sub- intra- or pre-retinal hemorrhage can obscure the visual axis and render permanent changes if not caught early or progresses to affect the entire retinal surface.
Extraocular and Miscellaneous causes

Feline restrictive orbital myofibroblastic sarcoma (FROMS)
Proper orientation and movement of the globe are essential for normal vision. Vision may be affected when there is severe globe deviation (strabismus) or erratic movement (nystagmus). Thankfully most types of strabismus and nystagmus found in cats are not severe enough to cause blindness as the brain can compensate for the most common ranges of these disorders. Certain acquired conditions affecting globe position in cats include feline restrictive orbital myofibroblastic sarcoma (left), or FROMS (also known as feline orbital pseudotumor), or traumatic orbital fibrosis from previous orbital infection, trauma, or inflammation, can render a globe blind simply from causing severe malorientation of the visual axis. CNS and optic nerve diseases can cause blindness without disturbing the ocular visual axis. Atrophy or hypoplasia of the nerve may develop in cats due to congenital malformation, trauma, certain infections (panleukopenia in kittens), or other ocular changes, including glaucoma, low blood pressure within the eye, retinal degeneration, or inflammation. Most of these changes are irreversible, but there may be no clues to this condition in some cats with unilateral changes other than a single dilated pupil. Optic neuritis in cats is the more common optic nerve cause for blindness and can sometimes be detected with a combination of visual reflex testing, direct or indirect fundoscopy, orbital imaging, and analysis of the CSF serology cytology and culture. Blood serology may also be helpful to screen for systemic involvement. As with retinal disease, cats may get optic neuritis from infection (toxoplasmosis, cryptococcosis, neospora), cancer (e.g., lymphoma), or autoimmune disease.
Every once in a while, you may get a cat that has a clear visual axis, normal globe orientation, and no CNS disease (normal visual reflexes), but still acts blind. Sciascopy, or retinoscopy could be done to evaluate for abnormal visual refraction and is typically found in pediatrics, veterinary university settings or in some veterinary ophthalmology practices. You may consider visual focusing problems (ametropia) or behavior issues as differentials for these patients. Corrective lenses are not available for cats (or dogs), but at least you have something to discuss with your client as a possible explanation for the poor vision when nothing else pans out.
Summary
Cats share some causes of blindness in dogs, but there are certain conditions that affect cats specifically and more frequently, including blindness from feline herpes keratitis, corneal sequestrum, hypertensive retinopathy, baytril toxicity, post-traumatic intraocular sarcoma, and FROMS. Diagnosing blindness in cats requires a good understanding of the components of the visual axis and the eye reflexes that govern it. Having the proper tools and access to the right tests are essential to localize the lesions present and formulate a plan and expectations for your clients.