-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 By Callie E. Cazlan, DVM (Emergency Veterinarian)
By Callie E. Cazlan, DVM (Emergency Veterinarian)![]()
angell.org/emergency
emergency@angell.org
617-522-5011
January 2021
Introduction/Indications for Blood Product Administration
The safe and proper administration of blood products can be one of the most critical life saving measures you will take during your shift. This article is targeted to veterinary technicians working in an emergency and critical care environment where these products are considered and administered with any frequency. In my clinical practice, the cases we will touch on here have been some of my most rewarding.
When a patient is triaged, there are some initial parameters that may clue you in to the need for blood product administration. Historical clues may include presenting signs of collapse, weakness, trouble getting up, anorexia, shallow breathing and/or exposure to toxins (rodenticide, onions, etc.). Patients presenting with pale gums, tachycardia (heart rate >160 bpm), bounding pulses, elevated respiratory rate (respiratory rate > 40 bpm) with a shallow breathing pattern are considered indications that a blood transfusion may be indicated. Recognizing these hemodynamic parameters and subsequently selecting the right blood product is critical in this moment. The veterinarian and technician must work together to make this selection to ensure the correct product is safely administered. Below is a table summarizing the most common types of blood products and case types where blood transfusion might be considered. In some cases multiple products may be indicated. Expanded component therapy is beyond the scope of this article.
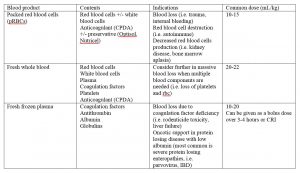
Table 1: Blood Products and Usage
Blood Types and Typing
Once a patient is selected as a candidate for a blood transfusion, the next question you will need to answer is the patient’s blood type. Knowing the proper blood type helps mitigate the risk of a transfusion reaction (covered below). Blood types are antigens present on the surface of the red blood cell membrane. Adverse reactions occur when the recipient has existing antibodies that are specific for antigens on the donor erythrocytes. In canines we use the dog erythrocyte antigen (DEA) typing system, with DEA 1.1 blood type being the group that is most likely to trigger a reaction if given to a 1.1 negative dog, and thus the most clinically relevant. A dog can be positive or negative for DEA 1.1. Several other blood types (3,4,5,7 and dal) are described in dogs but testing is not widely available for these groups at this time and have relatively low clinical relevance.
The two most utilized tests to determine DEA 1.1 status is the DMS card test (CARD, DMS Laboratories, NJ) and the Quick Test DEA 1.1 (CHROM, Alvedia, France). In the DMS card test, DEA 1.1 positive dogs will react with a lyophilized murine monoclonal antibody on the test card. The result of this reaction is strong hemo-agglutination (see example in picture 1). The cards also display a positive and negative control to ease interpretation. This test is considered rapid (<2 minute turnaround) and reliable. False negative results have been documented in patients with PCV <15%. Fortunately, this is ok for a first time transfusion as positive animals can tolerate a single negative transfusion as they lack preexisting alloantibodies. This may also be considered if blood typing is unavailable.
The Quick Test DEA 1.1 is an immunochromatographic cartridge system. It contains a membrane using a monoclonal antibody to the DEA 1.1 antigen. Capillary action under the influence of a buffer, results in migration of the erythrocytes to the membrane. DEA 1.1 positive red blood cells will be bound and retained resulting in a visible red band across the membrane. If no red band appears, then the patient is DEA 1.1 negative. This test is also considered rapid and can be used in patients exhibiting auto-agglutination (i.e. immune mediated hemolytic anemia).
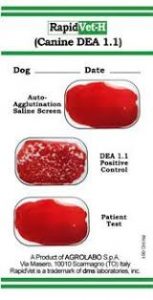
Picture 1: DEA 1.1 negative test result on DMS card typing system. https://www.megacor.at/useruploads/files/rapidvethcanine_en_web_3.pdf
Cross Matching and When To Do It
Now that you have the patient’s blood type, the question is do we need to cross match? The goal of cross matching is to determine if the patient is likely to have a hemolytic reaction to the blood product being administered. We must remember that the goal of any transfusion is to select a donor that will provide the maximum benefit but minimal harm to the patient. For a first-time transfusion in a dog, it is not standard to perform a cross match. There is some debate to this generalization but for the vast majority of transfusion naïve canine patients there is an absence of naturally occurring alloantibodies making a clinically relevant hemolytic transfusion reaction unlikely. Cross matching is absolutely indicated when the patient has received a blood transfusion in the past (roughly >4 days prior) or has an unknown transfusion history. This is based on the fact that it takes the body about 4 days to develop antibodies.
There is a major and minor cross match. A major cross match tests the recipient’s serum for alloantibodies against donor blood cells. A minor cross match tests the donor’s serum for alloantibodies against recipient blood cells. Most institutions perform major cross matching and commercial kits are available for point of care testing.
Blood Product Administration
Now let’s save some lives! Packed red blood cells and whole blood cells products generally do not need to be warmed prior to administration. Fresh frozen plasma should be warmed in a sealed plastic bag in a warm water bath prior to administration. Blood products should never exceed 98.6 F (37 C) as this may encourage bacterial growth and may cause protein denaturation.
Blood products are most commonly given via an intravenous route when possible. Intraosseous or peritoneal administration can be considered if IV access is not attainable. It is recommended that blood products are administered through a standard blood filter set (170-260 microns) to eliminate debris and blood clots from entering the recipient. It should be noted that the priming volume of these sets is too large for cats and small dogs (<10 kg). A human neonatal syringe filter set with a 150 micron filter or a syringe pump with a HemoNature (18 micron) filter can be considered as an alternative for these patients.
The veterinarian you are working with will give you a volume and rate of the blood product to the be administered. This can be determined by the guidelines outlined in table 1. The rate at which to administer the blood product will be determined by the clinical status of the patient. If a patient is rapidly losing blood (i.e. hemoabdomen) and is in danger of decompensating, the transfusion may be administered as quickly as a standard crystalloid fluid bolus (over 10-15 minutes). Alternatively, if a patient has a more stable disease process (i.e. immune mediated hemolytic anemia), the transfusion may be given over a few hours. The transfusion should never be given over >4 hours to prevent bacterial growth.
Lastly, if a patient needs ongoing support (i.e. oncotic with ongoing protein loss), a continuous rate infusion (CRI) of plasma may be considered. A common example of this would be a puppy with parvovirus that has low albumin from GI loss and thus is having trouble maintaining blood pressure. CRIs should be drawn up in no more than four-hour aliquots to be administered, again to prevent bacterial growth in the blood product. 45ml/kg of plasma can raise the albumin in the recipient by 1.0g/dL. If fresh frozen plasma is thawed and then not used it is able to be re-frozen within an hour without adverse effects.
Monitoring and Possible Reaction Types
Close monitoring is one of your most important roles as a technician in the course of a blood transfusion. The frequency of transfusion reactions of all types are generally low (3.3-15%). This is low enough that you should have confidence in the product but high enough that you should be vigilant in monitoring and be aware that a patient may need alteration in the chosen protocol for administration to mitigate any adverse effects.
At the start of a transfusion, all patients should have baseline vitals (temperature, heart rate, respiratory rate and capillary refill time) recorded. It is recommended that for the first 5-15 minutes of a transfusion the product is given at a half rate or 0.25 mL/kg/hr to evaluate for any initial reactions. After about 5 minutes, these vitals should be re-evaluated. If no reaction is documented then this should be repeated at 15, 30 and 60 minutes throughout the transfusion (individual hospital protocols may vary). It may be helpful to use a separate treatment sheet for transfusion monitoring during a transfusion procedure. This sheet may also include transfusion administration and donor information for the record. Additionally, the technician should be watching for signs of nausea, increased respiratory effort, changes in mentation, hematuria and restlessness as this may indicate an adverse reaction. In summary, if anything changes from your baseline, the veterinarian on the case should be notified.
Transfusion reactions can be divided into acute (up to 48 hours) and delayed reactions (beyond 48 hours). Acute reactions are divided into acute hemolytic and non-hemolytic reactions. The febrile non-hemolytic reaction is the most common reaction seen. Dogs who experience febrile non-hemolytic reactions can usually complete their transfusion but rates typically need to be slowed. This reaction may be indicated by fever, tachycardia, tachypnea, vomiting and diarrhea. For patients receiving plasma transfusions who develop urticaria and pruritis, diphenhydramine and steroid administration may be beneficial.
Hemolytic reactions are considered severe and are much more likely to be fatal. Good cross matching practice makes hemolytic reactions much less likely. Additional signs to watch for associated with this type of reaction include pigmenturia and cardiovascular collapse. If this type of reaction is suspected the transfusion should be stopped. Non-immunologic acute reactions can also occur. This can include transfusion-associated circulatory overload (TACO) which is simply a volume overload to the patient. This is standardly treated with a furosemide and stopping the trasnfusion. Additionally, patients can develop citrate toxicity. Citrate is used in anti-coagulated blood products and can chelate ionized calcium leading to hypocalcemia. This can cause tremors, facial pruritis, hypotension and arrhythmias. This can be treated with administration of intravenous calcium in a separate line.
Delayed reactions can be divided into shortened RBC lifespan (hemolysis), transfusion-related immunomodulation (TRIM) and infectious disease transmission. Responsible donor selection with thorough health screening prior to donation and cross matching can help avoid these complications. Unfortunately, TRIM can manifest as severe damage to the lungs, kidneys and other vital organs. These reactions are rare but often fatal when manifested. In any patient that develops additional clinical signs (dyspnea, collapse, vomiting) within days of a transfusion, this should be considered. Treatment is largely supportive.
Conclusions
In summary, blood products are a key component in the treatment of many of our most critical patients. Most often, blood products can be the support a patient needs while we buy time to stabilize his or her underlying disease process. Veterinarian technicians working in emergency and critical care should have a solid baseline knowledge of these principles and an enthusiasm to learn more and work with the patients that need these products.
Reference
- Callan MB, Oakley DA, Shofer FS, et al, Canine red blood cell transfusion practice. J Am Anim Hosp Assoc 1996;32:303-311
- Jamie M. Burkitt Creedon, H. D. (2012). Advanced Monitoring and Procedures for Small Animal Emergency and Critical Care. Ames: Wiley and Blackwell.
- Kenneth J. Drobatz, K. H. (2019). Textbook of Small Animal Emergency Medicine . Hoboken: Wiley and Blackwell.