-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Referrals
- Referral Forms/Contact
- Direct Connect
- Referring Veterinarian Portal
- Clinical Articles
- Partners in Care Newsletter
CE, Internships & Alumni Info
CE Seminar Schedule
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 Sandra Alleiler, DVM, DACVA, DMVA, CCRT
Sandra Alleiler, DVM, DACVA, DMVA, CCRT![]()
angell.org/anesthesia
anesthesia@angell.org
617-541-5048
2022
Risk factors for anesthetic-related death in cats
Endotracheal intubation has been identified as a risk factor for anesthesia-related morbidity and mortality in cats. Results from the confidential inquiry into perioperative small animal fatalities (EPSAF) (Brodbelt et al. 2007) have shown that between June 2002 and June 2004, 175 deaths were classified as anesthetic and sedation related. During the study, 79,178 anesthetic and sedation procedures were recorded, and the overall risk of anesthetic and sedation-related death was 0.24% (95% CI 0.20–0.27). Factors associated with increased odds of anesthetic-related death were poor health status (ASA physical status classification), increasing age, extremes of weight, increasing procedural urgency and complexity, endotracheal intubation, and fluid therapy. Pulse monitoring and pulse oximetry were associated with reduced odds.
What makes cats more difficult for orotracheal intubation?
Feline airways are small and more sensitive to trauma, spasm, and edema than other species. The glossoepiglottic frenulum runs from the dorsal surface of the tongue to the cranial aspect of the epiglottis. Pulling the tongue rostrally moves the tip of the epiglottis forward and down, exposing the laryngeal inlet and vocal cords.
Proper airway management is essential for safe anesthesia in cats. General anesthesia is associated with loss of protective airway reflexes and respiratory depression. The importance lies in maintaining a patent airway and supporting ventilation when required. Most anesthetic-related deaths occur after premedication during an induction or soon after anesthesia ends (within the first three hours) and are commonly caused by airway obstruction.
Laryngospasm
 Cats are prone to laryngospasm, characterized by tight closure of the arytenoids in response to mechanical or chemical stimulation. Laryngospasm can occur during intubation as well as during extubation. It is rare for it to happen later during recovery. Applying 0.1 ml lidocaine 2% onto the arytenoid cartilages can blunt the spasm. Thirty seconds should be allowed for the local anesthetic to take effect. Propofol, alfaxalone, sedatives, and neuromuscular blocking agents can reduce the occurrence of laryngospasm.
Cats are prone to laryngospasm, characterized by tight closure of the arytenoids in response to mechanical or chemical stimulation. Laryngospasm can occur during intubation as well as during extubation. It is rare for it to happen later during recovery. Applying 0.1 ml lidocaine 2% onto the arytenoid cartilages can blunt the spasm. Thirty seconds should be allowed for the local anesthetic to take effect. Propofol, alfaxalone, sedatives, and neuromuscular blocking agents can reduce the occurrence of laryngospasm.
Necessary equipment and methods
A laryngoscope to visualize the rima glottidis (space between the vocal ligaments). The laryngoscope should have a long enough blade to allow correct placement at the base of the epiglottis. It should not touch the epiglottis. The light needs to be checked to be in good working order and bright. Using the flashlight from a smartphone can add an extra light source.
Endotracheal tubes
Endotracheal tubes come in a wide range of internal diameters. Endotracheal tubes with cuffs provide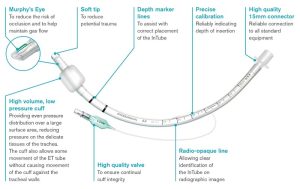 a secure airway; there is no leakage of oxygen or inhalation of anesthetic agents when the cuff is inflated, which allows ventilation, and placement can be confirmed by visualization between arytenoids. Disadvantages are: requiring skills and a deeper plane of anesthesia, traumatic injury and tracheal damage can occur. Overinflation of the cuff can cause necrosis or tear of the trachea. Endotracheal tubes uncuffed provide a patent airway, reduce the risk for tear, and visualize placement. They do not protect from aspiration; inhalation anesthetic leaks around the tube during spontaneous breathing and mechanical ventilation.
a secure airway; there is no leakage of oxygen or inhalation of anesthetic agents when the cuff is inflated, which allows ventilation, and placement can be confirmed by visualization between arytenoids. Disadvantages are: requiring skills and a deeper plane of anesthesia, traumatic injury and tracheal damage can occur. Overinflation of the cuff can cause necrosis or tear of the trachea. Endotracheal tubes uncuffed provide a patent airway, reduce the risk for tear, and visualize placement. They do not protect from aspiration; inhalation anesthetic leaks around the tube during spontaneous breathing and mechanical ventilation.
Endobronchial intubation is possible if the ET tube is pushed beyond the thoracic inlet. Regardless of what type or size of an endotracheal tube is used, the length should correspond to the distance between the patient’s incisors and the point of the shoulder (thoracic inlet). Stylets can increase stiffness in the floppier silicone tubes, but the tip should be blunt and remain within the lumen of the endotracheal tube.
Additional equipment
Cotton-tipped applicators can be helpful to clear mucus and saliva, but a suction unit should be readily available to clean excess saliva, which often occurs in patients with upper respiratory tract obstruction. A urinary catheter with a 3.5 mm internal diameter ETT connector attached can be used as a stylet or to provide oxygen. A bougie is a flexible device made of braided polyester with a resin coating. It can be used instead of a urinary catheter to guide the ETT. The advantage is that it is more rigid than a urinary catheter and may be easier to place. The disadvantage is that the capnograph or oxygen supply cannot be connected unless a special bougie with a central lumen and port for ventilation is used.
V-gel: Supraglottic airway devices
 This device does not enter the trachea and ends above the larynx. They are specifically designed for the cat’s pharyngeal and laryngeal anatomy. Studies have shown that the time to obtain a clinically acceptable capnograph reading is shorter when a supraglottic airway device was used compared with an ETT, fewer attempts were needed, and less propofol was required. Disadvantages are that correct placement cannot be confirmed by visualization, changes in patient position can easily dislodge the device, and it may take up to much room for oral procedures. Supraglottic airway devices are not recommended if abnormal laryngeal anatomy is present.
This device does not enter the trachea and ends above the larynx. They are specifically designed for the cat’s pharyngeal and laryngeal anatomy. Studies have shown that the time to obtain a clinically acceptable capnograph reading is shorter when a supraglottic airway device was used compared with an ETT, fewer attempts were needed, and less propofol was required. Disadvantages are that correct placement cannot be confirmed by visualization, changes in patient position can easily dislodge the device, and it may take up to much room for oral procedures. Supraglottic airway devices are not recommended if abnormal laryngeal anatomy is present.
Fiber-optic-assisted intubation
Fiber-optic intubation (FOI) is an effective technique for establishing airway access in patients with anticipated and unanticipated difficult airways. First described in the late 1960s, this approach facilitated airway management and was added to ASA guidelines for managing difficult airways.
Video laryngoscopy (VL) is a form of indirect laryngoscopy in which the clinician does not directly view the larynx. Instead, visualization of the larynx is performed with a fiber-optic or digital laryngoscope inserted trans-nasally or transorally. Images are magnified, allowing for a detailed examination of the larynx. The images from video laryngoscopy can be displayed on a monitor and recorded.
Fiber-optic intubation involves threading an endotracheal tube over a flexible fiber-optic scope shaft. The scope is passed through the mouth or nose into the pharynx and through the vocal folds into the patient’s trachea. Upon visual confirmation of tracheal rings and carina, the fiber-optic scope is held steady while the ET tube is advanced over the fiber-optic bundle into the airway. Once the tube is in place, the scope is removed.
A new simple, fast and safe oral intubation technique for rats, which is very similar to VL for intubation in humans, has been described using a cost-effective, commercially available device for ear wax removal in humans. It may help in difficult cat intubations, but future research is warranted.
Veterinary video otoscopes that connect to an iPhone/iPod, using its camera technology to provide a high-definition image of the anatomy, have also been used for intubation. The dual-channel for flushing and removing foreign objects such as foxtails can be used to guide a urinary catheter as a stylet through the vocal folds and advance the ET tube quickly and easily. This technique has been used and facilitates intubation in rabbits and other pocket pets and may also have a place in cat intubation.
Clinical airway management continues to advance at a fast pace. Devices produced over the last 30 years have transformed airway management in human medicine, and it is only a question of time and skills until they will become readily available in veterinary medicine.