-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 By Steven Tsai, DVM, DACVR
By Steven Tsai, DVM, DACVR
angell.org/diagnosticimaging
617-541-5139
Diagnostic x-ray studies are ubiquitous in veterinary healthcare facilities, and with the rise of digital radiography, the ease of acquiring images is exponentially improved relative to the era of hard film, chemical developers, and dark rooms. With the near-instantaneous availability of a review image following exposure, repeat exposures are easy and effectively free of cost. The hidden cost, however, is increased radiation exposure.
X-rays are high energy photons which can pass through materials and often collide with atoms in the body, potentially removing orbital electrons (ionization). Damage can affect DNA directly (less common) or indirectly through interaction with water and creation of free radicals (more common). While the cellular DNA repair mechanism is quite reliable, it is not perfect, and failure to repair DNA damage correctly can lead to a mutation, which may lead to cancer.
Although the risk of developing cancer from a single x-ray exposure is small, current epidemiological data suggest that there is no minimum threshold below which there is zero risk of cancer. Additionally, this risk is considered to be cumulative over a person’s lifetime. A 2004 study estimated the attributable risk for a US resident of developing cancer due to medical x-ray exposure to be 0.9%, resulting in 5695 cancer deaths per year.1 Therefore, reducing radiation exposure as much as possible (As Low As Reasonably Achievable, or ALARA) is the guiding principle.
The three factors in minimizing radiation exposure to veterinary personnel are Time, Distance, and Shielding.
Time — Reduce the amount of time exposed to radiation. Generally speaking, this means trying not to be in the room at all during exposure. Experienced radiology technicians generally achieve this by using either tape or sandbags to hold the patient in place while they run out of the room for the exposure. Judicious use of chemical sedation for x-ray studies also greatly improves ease of acquisition and reduces stress both for the patient and for the techs. In some states, it is actually illegal for a human to be in the room during x-ray exposure for a veterinary patient.
Distance — Radiation levels decrease with distance according to the inverse square law, which is to say it decreases exponentially as you move away from the source. Thus, even small increases in distance can result in significant drops in exposure. Generally speaking, exposure is considered to be effectively zero if you are >6 feet away from the x-ray source.
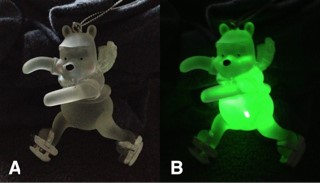
Image 1 — A. Frosted glass ornament. B. Laser pointer aimed at the belly. Note that the entire ornament, from the ears to the distal extremities, glows with green light, even with just a pinpoint exposure to the primary beam. This is analogous to how a patient scatters the x-ray beam.
Shielding — If you must be in the room for exposure, lead shielding is imperative. At minimum, a lead apron, thyroid shield, and lead gloves should be worn. A common misconception is that adequate hand protection can be achieved by draping a lead glove over your hand while you directly grasp the patient’s leg. This is not adequate protection since the primary cause of radiation exposure to personnel is scatter (assuming the personnel is not within the primary x-ray beam), and the primary source of scattering is not the x-ray tube, but the patient itself! Since the patient is not 100% transparent to x-rays, some of the x-rays inevitably are scattered within the body and bounce around, sometimes exiting the body in a completely random direction. Effectively, the patient is “glowing” with scattered x-rays, so the hand holding the patient’s limb is directly exposed to the x-ray “glow” coming from the patient (Image 1). Thus, your hands should always be inside the lead glove, not just underneath it.

Image 2 — A. Poor quality image of the antebrachium with wide-open collimation. The loss of detail is attributable almost entirely to scatter. B. Same patient, with same exposure parameters, but appropriate collimation.
Tight collimation to the body part of interest also reduces scatter radiation, with the added bonus of improving image quality. Since x-rays pass through and are scattered by the materials they reach, a wide, open beam results in a large amount of excess scattered radiation. If you imagine a flashlight pointing at a disco ball, a wide beam of light which hits the whole disco ball scatters a great deal of light throughout the room, while a tightly focused beam of light would not result in nearly as much scattered ambient light. Scattered x-rays are also captured by the digital detector and result in noise and blurriness. (Image 2) Thus, more focused collimation reduces room scatter and improves image quality.
Medical x-ray use has greatly improved our diagnostic capabilities over the past century, and their use is steadily increasing with the advent of digital radiography and spread of teleradiology. It is crucial that all veterinary healthcare personnel who are involved with ordering or performing x-ray studies be aware of the potential risks and employ appropriate techniques to minimize radiation exposure to medical personnel.
Reference
- Risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries. de González, Amy Berrington et al. The Lancet , Volume 363 , Issue 9406 , 345 – 351.