-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 By Jessica Riehl, DVM, DAVDC
By Jessica Riehl, DVM, DAVDC![]()
angell.org/dentistry
dentistry@angell.org
617-522-7282
October 2023
x
x
Cone beam computed tomography (CBCT) is a relatively newer imaging modality to veterinary dentistry. Although this method has been available and highly used in human dentistry for many years, it was first evaluated for veterinary purposes only a decade ago. Since then, advancements have been made to make it a successful method for evaluating dental and maxillofacial anatomy. CBCT permits a three-dimensional evaluation of structures and multi-planar views. It has become extremely useful for assessing endodontic disease, maxillofacial trauma, and oncologic disease.
CBCT varies from traditional conventional computed tomography (CT) in a number of ways that are well-suited for veterinary dentistry. Whereas in conventional CT, when a fan-shaped X-ray beam is emitted, and the patient needs to be moved through the gantry, with CBCT, the X-rays are cone-shaped, and the machine rotates around a stationary patient. The X-ray source in CBCT comes from a flat source, which is opposite of the sensor. These characteristics allow the CBCT to operate with only one pass around the patient, and the patient receives very low radiation. The design of most CBCT machines is smaller and allows them to be transported or moved for convenience.
Imaging of the maxillofacial region has previously been accomplished by dental radiographs, skull radiographs, and conventional/helical computed tomography. Each of these methods has its advantages and disadvantages.
Dental radiography has been the standard of care since it is easily available, several options exist (DR, CR, a variety of software), has a reasonable price point, and provides extremely valuable clinical information. It evaluates the dentition and the bone surrounding the teeth, allowing the user to evaluate both periodontal and endodontic aspects. The X-rays are focused on a small area, and there is a relatively low overlap of other structures. Interpretation can be more challenging in brachycephalic patients due to their anatomy, with crowding and rotation of teeth expected. Dental radiograph use for evaluating maxillofacial structures as a whole is limited.
Skull radiographs will give a more global view to the user when looking at maxillofacial structures and evaluating for maxillofacial trauma (i.e., fractures). The downsides are that diagnostic skull radiographs can be challenging to obtain without an experienced user performing positioning (appropriate marking necessary, right and left obliques, dorsal-ventral, and rostrocaudal views all necessary), and interpretation can be challenging. The difficulty in interpretation arises from the superimposition and overlapping of structures, which can make them of limited use. For quality images, patients need to be sedated to obtain skull radiographs.
Magnetic resonance imaging (MRI) can be useful when evaluating soft tissue structures of the head; however, its ability to assess dental or maxillofacial bone is inadequate.
As previously mentioned, standard computed tomography provides 3-D imaging of the maxillofacial region and is commonly available at multi-specialty hospitals. The generator rotates around the patient as the patient moves through the gantry. The captured images overlap slightly, and computer software transforms the data into 3-D images. CT eliminates the issue of superimposition when evaluating the maxillofacial structures. It can be used to evaluate hard tissue (teeth and bone) and soft tissue. Additionally, with the use of contrast, certain features can be enhanced (areas of inflammation or increased vascularity). The price of these units, the need for an experienced technician to perform scans, dedicated floor space, and requirements for appropriate radiation safety make this modality impractical for general use.
Similar to standard CT, CBCT eliminates the problem of superimposition of structures, creates a 3-D reconstruction of the area of interest, and allows evaluation of dentition and bone. CBCT has the capability to provide increased detail of the dentoalveolar structures due to thinner slices and better resolution. Compared to standard CT, which will obtain a slice (image) every 1 to 3 mm, CBCT slice thickness is 0.1 to 0.4 mm. This is a great advantage when evaluating dental structures. Previous studies have indicated that CBCT was superior in image quality compared to standard CT when assessing enamel, dentin, pulp cavity, periodontal ligament space, lamina dura, and trabecular bone.
Clinically speaking, the greatest advantage of adding CBCT in veterinary dentistry patients comes from the ability to see anatomy in a 3-D nature. Compared to our two-dimensional radiographs, CBCT eliminates missing or misinterpreting pathology since overlapping structures are eliminated. The sensitivity of CBCT to demineralization of bone permits a periapical lesion to be detected sooner than visible changes can be identified on a dental radiograph, therefore allowing endodontic disease to be picked up sooner. The risk for complications from extractions is also minimized when using CBCT as it allows more information on the positioning of roots to neighboring vital structures (e.g., mandibular canal, infraorbital canal, nasal cavity, or sinuses). Surgical approach and expectations on what may be encountered can also allow a better-informed clinician, particularly if there is a structural abnormality to a root, such as dilaceration to the root end.
Dental radiographs will likely continue to remain the standard of care for dentistry, with CBCT as an ancillary technique used at the specialist level. Specific indications for CBCT include evaluating maxillofacial trauma (i.e., jaw fractures), temporomandibular joint disease, brachycephalic patients (with crowding and rotation of teeth), cystic lesions (i.e., dentigerous cyst), palatal defects, or bony tumor involvement. In the future, manufacturers will likely work on different software versions with algorithms to better evaluate soft tissue.
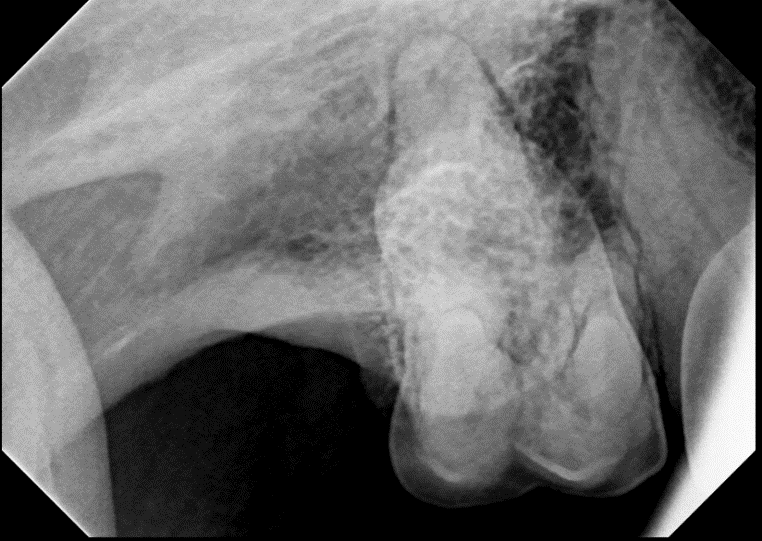
Figure 1. Dental radiograph of the right maxillary first molar (109) using standard bisecting angle technique.
x
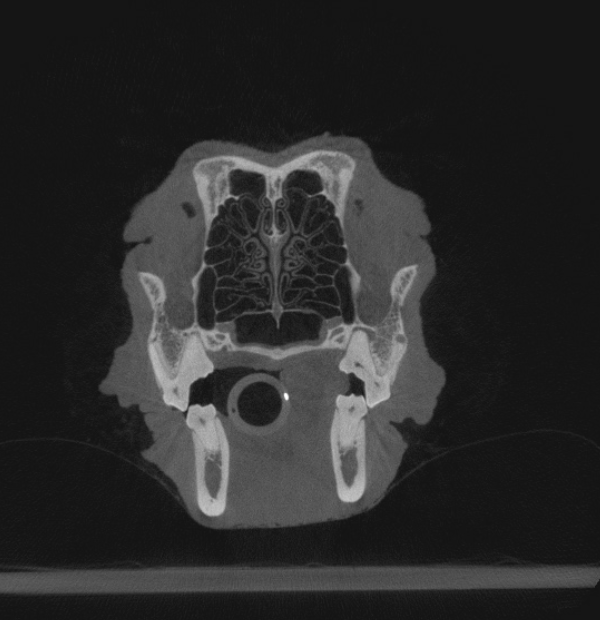
Figure 2. Same patient as Figure 1. Axial image obtained from CBCT at the level of the maxillary first molars. The patient’s right side is on the right side of the image. Note the periapical lucency associated with the mesiobuccal and palatal roots of the right maxillary first molar (109), which are not easily identified on the previous radiograph.
x
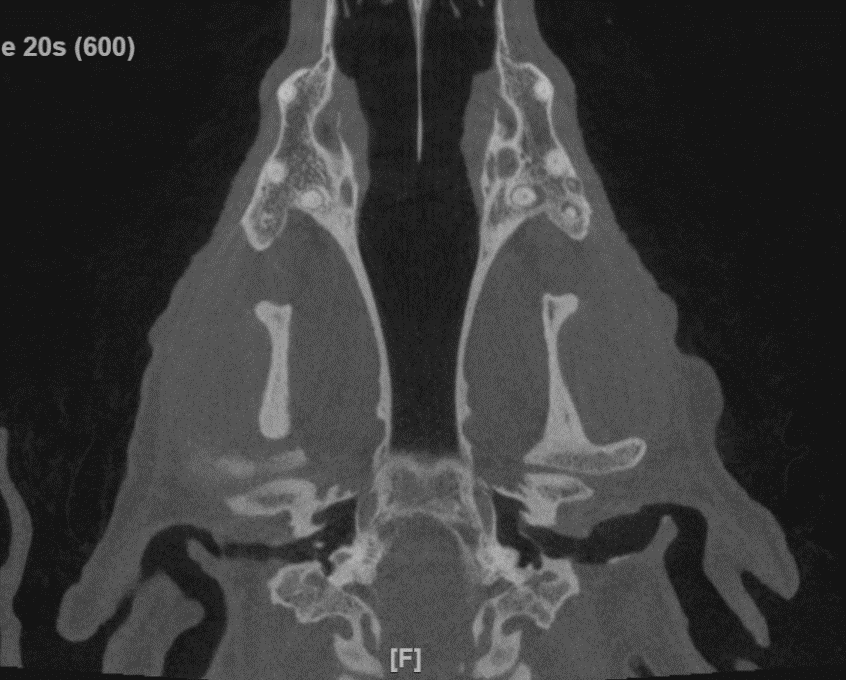
Figure 3. Same patient as Figures 1 and 2. Coronal view obtained from CBCT at the apical region of the maxillary fourth premolars and first molars. The patient’s right side is on the right side of the image. The widened periodontal ligament space and periapical lucencies around the mesiobuccal, distobuccal, and palatal roots of the right maxillary first molar (109) can be identified. The proximity of the mesiobuccal root of 109 to the distal root of the maxillary fourth premolar (108) can also be appreciated.
x
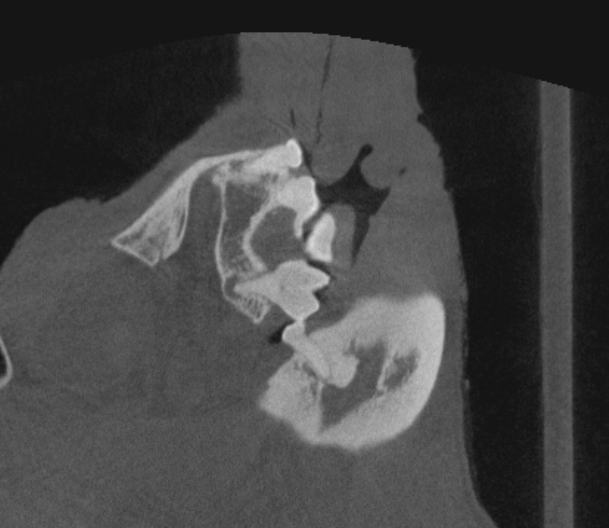
Figure 4. Same patient as Figures 1, 2, and 3. Sagittal view from CBCT images at the level of the palatal root of the right maxillary first molar (109). A periapical lucency is clearly defined around the root apex, indicating endodontic disease, leading to the decision for surgical extraction of the tooth.
x
x
References
- Van Thielen, Bert, et al. “Cone beam computed tomography in veterinary dentistry.” Journal of Veterinary Dentistry 29,1 (2012): 27-34.
- Villamizar-Martinez, Lenin A, and Anson J Tsugawa. “Diagnostic Imaging of Oral and Maxillofacial Anatomy and Pathology.” The Veterinary clinics of North America. Small Animal Practice 52,1 (2022): 67-105.
- Roza, Marcello R et al. “Cone beam computed tomography and intraoral radiography for diagnosis of dental abnormalities in dogs and cats.” Journal of Veterinary Science 12,4 (2011): 387-92.
- Berning, Jamie A et al. “Analysis of the Anatomic Relationship Between the Mandibular First Molar Roots and Mandibular Canal Using Cone-Beam Computed-Tomography in 101 Dogs.” Frontiers in veterinary science 6 485. 17 Jan. 2020.
- Heney, Colleen M et al. “Diagnostic Yield of Dental Radiography and Cone-Beam Computed Tomography for the Identification of Anatomic Structures in Cats.” Frontiers in Veterinary Science 6 58. 28 Feb. 2019.
- Döring, Sophie, et al. “Evaluation of the diagnostic yield of dental radiography and cone-beam computed tomography for the identification of dental disorders in small to medium-sized brachycephalic dogs.” American Journal of Veterinary Research 79,1 (2018): 62-72.
- Döring, Sophie, et al. “Evaluation of the diagnostic yield of dental radiography and cone-beam computed tomography for the identification of anatomic landmarks in small to medium-sized brachycephalic dogs.” American Journal of Veterinary Research 79,1 (2018): 54-61.
- Soukup, Jason W et al. “Comparison of the Diagnostic Image Quality of the Canine Maxillary Dentoalveolar Structures Obtained by Cone Beam Computed Tomography and 64-Multidetector Row Computed Tomography.” Journal of Veterinary Dentistry 32,2 (2015): 80-6.