-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 By Ruth Van Hatten, DVM, DACVR
By Ruth Van Hatten, DVM, DACVR
diagnosticimaging@angell.org
617-541-5139
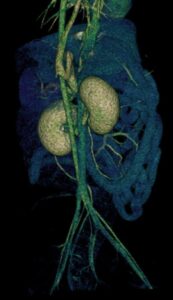
Fig 1. 3D image of CT angiography demonstrating a single congenital extrahepatic portosystemic shunt extending from the portal vein to the azygos vein.
Cross-sectional imaging has become a mainstay in veterinary imaging, and what was once considered unavailable or too expensive is now widely used on a daily basis. CT and MRI have allowed veterinarians to drastically improve the quality of care, and with pet insurance being more commonplace, they are no longer considered unaffordable. The purpose of this article is to compare the pros and cons of CT and MRI and discuss the various indications in which one modality would be recommended over the other.
Computed Tomography (CT) uses numerous x-ray beams in a helical format surrounding the patient in order to create a 3D image. CT uses ionizing radiation that is approximately 10 times that of a comparable radiographic study. This does impose a greater risk of DNA damage compared to radiographs; however, the benefits greatly outweigh these risks when indicated, and it is generally accepted that the shorter life expectancy of our domestic pets decreases the chances of long term side effects of radiation exposure. Compared to MRI, CT is very quick and has become even faster with increased slices and newer models. This has allowed for some studies to be performed under heavy sedation instead of general anesthesia, specifically emergency cases where the patient is too unstable to undergo general anesthesia and routine musculoskeletal exams (for example, evaluation for elbow dysplasia). Abdominal CT has been shown to detect more lesions in dogs greater than 25kg compared to abdominal ultrasound because the larger size of the patients and gastrointestinal gas hampers complete visualization of all organs on ultrasound. In addition, thoracic CT has been shown to better detect pulmonary nodules compared to radiography.
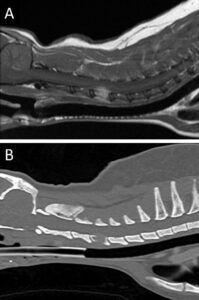
Fig 2. MRI of the neck in T1w plus contrast (A) and a CT in bone algorithm (B) in the sagittal plane. The T4 vertebral body contains an expansile tumor resulting in lysis of the bone and secondary compression of the spinal cord.
With power contrast injectors and the use of high slice CT machines, three phase angiograms can be performed. This allots improved surgical planning as arteries can be differentiated from veins and the vascular anatomy has better resolution. Three phase CT angiograms have been used to evaluate for vascular anomalies such as portosytemic shunts, aortic arch malformations, arteriovenous malformations, and anomalous coronary arteries. In addition, three phase studies have been shown to increase detection of insulinomas and certain metastatic lesions within the abdomen.
CT has improved soft tissue contrast compared to radiographs and is excellent for evaluating the bone. CT is the gold standard for evaluating trauma cases, as patients can be scanned quickly with improved diagnosis of subtle fractures compared to radiographs. CT has been shown to have a sensitivity of up to 100% for detecting acute bone lesions. In evaluating complex pelvic fractures and imaging the skull, CT is recommended as superimposition on radiographs greatly effects thorough evaluation.
Magnetic Resonance Imaging (MRI), in contrast, uses radio waves and a magnetic field in order to create a 3D image. It is overall considered very safe and does not utilize ionizing radiation. Because a magnetic field is involved in creating the image, the main risk factors are projectiles secondary to the strong magnetic field and possible motion and heating of ferromagnetic objects within the body (e.g. metallic implants). It is important to note that this is considerably more of a concern in human medicine where patients commonly have pacemakers and aneurysmal clips. MRI is significantly longer compared to CT and general anesthesia is required as motion while imaging results in significant artifacts. In addition, the cost of an MRI scan can be two to three times that of a CT scan.
So when is MRI better than CT? MRI is considered the gold standard for neuroimaging. MRI allows superb soft tissue contrast allowing differentiation between grey and white matter within the brain and spinal cord. Thus for any patient with neurologic deficits, MRI is generally recommended over CT. The few instances where CT can be used over MRI are with suspected middle ear disease resulting in peripheral vestibular signs and in some cases of suspected intervertebral disc displacement (as mineralized displaced discs can be visualized on CT). One report showed that only approximately 8% of patients that have undergone CT for thoracolumbar myelopathy required additional imaging to come to a diagnosis. Despite CT having good diagnostic capability, MRI is overall more sensitive and accurate than non-contrast CT for diagnosis of intervertebral disc herniation, and thus MRI remains the gold standard. In evaluating intracranial disease, MRI has improved imaging for inflammatory lesions compared to CT, but one report documents that CT is similar to MRI in measuring brain tumors (specifically gliomas). MRI has been shown to better detect meningeal enhancement and have a greater measured tumor volume compared to CT in dogs with nasal tumors. With the superior soft tissue contrast, MRI also grants greater visualization of tendons and ligaments compared to CT. Imaging of canine joints (specifically shoulder and stifle) with MRI allows improved diagnosis of tendon and ligament injuries and is commonly used in human medicine to evaluate soft tissue injuries.
In some cases, both MRI and CT are used concurrently to obtain the most information to develop a complete treatment plan, specifically, trauma cases where fractures are suspected with concurrent neurologic deficits. MRI would be recommended to thoroughly evaluate the spinal cord and structural soft tissues of the vertebral column for injury as well as acute, traumatic disc displacement. MRI can detect inflammation in and around bone, but CT would be recommended to better evaluate the bone margins for fractures and fissure lines, in addition to surgical planning. Another example includes malformations resulting in neurologic deficits that require surgical intervention (for example, vertebral malformations such as kyphosis).
Veterinary medicine has come a long way with improvements in cross-sectional imaging. When determining which modality would be recommended, many factors must be considered including patient size, stability, clinical differential diagnosis, and experience/comfort level. The future holds improved soft tissue resolution with thoracic and abdominal MRI compared to CT with the use of respiratory and cardiac gating to eliminate associated motion artifacts. As new developments and technology become more readily available, in both CT and MRI, improved diagnostic capability is inevitable.
References
- Armbrust LJ, et al. JAVMA 2012;240(9):1088-1094
- Cooper JJ, et al. VRU 2014;55(2):182-189.
- Emery L, Hecht S, and Sun X. VRU 2018;59(2):147-154.
- Fields EL, et al. VRU 2012;53(5):513–517.
- Gallastegui, A, et al. VRU 2019;60(5):533-542.
- Hansen SC, et al. J Vet Emerg Crit Care (San Antonio) 2019;29(3):301-308.
- Lux CN, et al. VRU 2017;58(3):315-325.
- Robertson I and Thrall DE. VRU 2011;52(1 Suppl 1):S81-84.
- Stadler KL, et al. Front Vet Sci 2017;25(4):157