-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 by Maureen C. Carroll DVM, DACVIM
by Maureen C. Carroll DVM, DACVIM
www.angell.org/internalmedicine
internalmedicine@angell.org
617-546-5186
The more we learn about the etiology and pathogenesis of protein-losing nephropathy, the more drugs we have to choose from to target the varying conditions that lead to this disorder. Ten years ago we used ACE inhibitors and low protein diet to manage these cases. Today we have a number of medications from which to choose, alone or in combination, to better manage this disease.
Angiotensin converting enzyme inhibitors:
ACE inhibitors block the conversion of angiotensin I to angiotensin II, thereby helping the kidneys in several ways. These medications decrease glomerular transcapillary hydrostatic pressure, they preserve GBM heparin-sulfate and slit diaphragm, they decrease Aldosterone synthesis (which is beneficial/see below) and they help to minimize mesangial injury. The two medications most commonly used are:
* Benazepril: .25- .5 mg/kg q 12-24 hr
* Enalapril: .25-1 mg/kg q 12-24
Monitoring should include a blood pressure and renal panel PRIOR to initiation of therapy, followed by the same one week later, then ideally every 3 months.
Angiotensin receptor blockers
This class of medication selectively blocks type I angiotensin receptors, but leaves the type 2 receptor unopposed. The beneficial result is maintenance of renal vasodilation. By selectively blocking the AT1receptor, aldosterone synthesis and secretion is reduced causing vasodilation and decreased potassium and increased sodium excretion. While plasma concentrations of renin and angiotensin-II are increased, this does not counteract the blood pressure lowering effects. The end result is diminished proteinuria, elimination of inflammatory cell infiltration, amelioration of glomerular, and tubular structural change.
* Losartan: .25- 2mg/kg a 12-24 hours
* Irbesartan: This drug does not need to be converted to an active metabolite as does Losartan. Dogs may not convert Losartan to the active metabolite. Dosage: 5 mg/kg/day
Combination ACEI and ARB: maximizes blockade of the renin-angiotensin system by affecting both the bioavailability of angiotensin II and also by affecting its activity at the receptor level. This combination might be considered with refractory/progressively worsening proteinuria.
Aldosterone inhibitors:
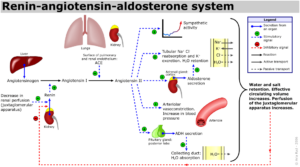
This class of medication selectively inhibits the actions of aldosterone (see Figure 1), independent of renin-angiotensin blockade. Studies have shown that selective re-infusion of aldosterone RESTORES proteinuria and glomerular lesions DURING blockade of renin- angiotensin system. This suggests an independent pathogenic role for aldosterone as a mediator of progressive renal disease. Aldosterone also has fibrogenic properties in the kidney via TGF synthesis up regulation, another reason to consider blockade of its negative effects in the glomerulus. The medication most commonly used is spironlocatone, however this medication used in conjunction with ACEI may have a greater renoprotective effect.
* Spironolactone 1-2 mg/kg BID
Antithrombotics:
*The Coagulation system plays a role in the development of glomerular lesions‑notably intraglomerular coagulation and fibrin deposition. Platelets in particular may be involved in mediating/amplifying glomerular injury by promoting proliferation of glomerular mesangial and endothelial cells, increasing vascular permeability thereby facilitating glomerular localization of circulating immune complexes, promoting proteinuria via platelet-derived cationic secretory proteins leading to loss of glomerular negative charge and therefore enhanced capillary permeability. There is also a link between increased platelet destruction, proliferation of mesangial cells and glomerular inflammation due to platelet derived chemotactic factors for inflammatory cells.
* Low dose aspirin: 2 mg/kg day dogs; 5 mg /day cats
* Clopidogrel: 1-2 mg/kg once daily (dogs)
* Low molecular weight Heparin
- Fragmin 150 U/kg TID
- Lovenox .8-1 mg/kg SQ QID
Rivaroxaban is a medication used more commonly in humans for the prevention and TREATMENT of thrombosis. This medication targets free Factor X and clot-bound factor X specifically by inhibiting both free Factor Xa and Factor Xa bound in the prothrombinase complex. It is a highly selective direct Factor Xa inhibitor with oral bioavailability and rapid onset of action.
Inhibition of Factor Xa interrupts the intrinsic and extrinsic pathway, inhibiting both thrombin formation and development of thrombi.
2 mg/kg BID in dogs
Antihypertensives: Up to 80% of GN dogs are hypertensive which is associated with sodium retention, vascular fibrosis, impaired release of renal vasodilators, activation of the RAA system. Calcium channel blockers are the most commonly used medications in conjunction with ACE inhibitors. This class of medications dilates the afferent arteriole, and balances the effects of an ACEI on the efferent arteriole, thereby balancing the pressure gradient balanced across the glomerulus.
* Amlodipine .1- .5 mg/kg once daily
Immunosuppressant: Usage of these medications is ideally based on histopathology of the kidney. There are various protocols for various conditions, a topic too large to comprehensively cover here. In addition to corticosteroids, medications for consideration include: Cyclosporine, azathioprine, mycophenolate, Cyclophosphamide, and chlorambucil, among others.
- Omega 3 Fatty acids: These medications are renoprotective and can slow the progression of renal failure by limiting the production of or action of cytokines and eicosanoids evoked by the initial immunologic renal injury.
Goal: 150 mg/kg/day for renal patients
For more information, please contact Angell’s Internal Medicine service at 617-541-5186 or internalmedicine@angell.org.
References
- Chou J, Wunschmann A, Hodzic E, et al. Detection of Borrelia burgdorferi DNA in tissues from dogs with presumptive Lyme borreliosis. J Am Vet Med Assoc 2006;229:1260–1269.
- Dambach DM, Smith CA, Lewis RM, et al. Morphologic, immunohistochemical, and ultrastructural characterization of a distinctive renal lesion in dogs putatively associated with Borrelia burgdorferi infection: 49 cases (1987–1992). Vet Pathol 1997;34:85–96.
- Gerber B, Eichenberger S, Haug K, et al. Association of urine protein excretion and infection with Borrelia burgdorferi sensu lato in Bernese Mountain dogs. Vet J 2009;182(3):487–488.
- Gerber B, Haug K, Eichenberger S, et al. Follow up of Bernese Mountain dogs and other dogs with serologically diagnosed Borrelia burgdorferi infection: what happens to seropositive animals? BMC Vet Res 2009;5:18.
- Goldstein RE. Current understanding of Lyme nephropathy. Proc 25th ACVIM Forum 2007;672–673.
- Goldstein RE, Cordner AP, Sandler JL, et al. Microalbuminuria and comparison of serologic testing for exposure to Borrelia burgdorferi in nonclinical Labrador and Golden Retrievers. J Vet Diagn Invest 2007;19:294–297.
- Lees, GE, Brown SA, Elliott J, et al. Assessment and management of proteinuria in dogs and cats: 2004 ACVIM forum consensus statement (Small Animal). J Vet Intern Med 2005;19:377–385.
- Littman MP. Protein losing nephropathy. In: Acierno MJ, Labato MA (eds.) Kidney Disease and Renal Replacement Therapies. Vet Clin N Am (Small Animal) 2011:41(1):31–62.
- Littman MP, Goldstein RE, Labato MA, Lappin MR, Moore GE. ACVIM small animal consensus statement on Lyme disease in dogs: diagnosis, treatment, and prevention. J Vet Intern Med 2006;20(2):422–434.