-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Referrals
- Referral Forms/Contact
- Direct Connect
- Referring Veterinarian Portal
- Clinical Articles
- Partners in Care Newsletter
CE, Internships & Alumni Info
CE Seminar Schedule
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 By Daniel Biros, DVM, DACVO
By Daniel Biros, DVM, DACVO
![]() angell.org/eyes
angell.org/eyes
ophthalmology@angell.org
617-541-5095
November 2023
x

Managing a squinty dog is not always a straightforward endeavor.
x
What are the three most common eyelash anomalies?
Trichiasis is the most common eyelash irregularity, with ectopic cilia and distichiae occurring less frequently. However, distichiae and ectopic cilia are still recognized as more clinically severe disorders in contrast to trichiasis due to their overall increased morbidity. All three abnormalities can potentially cause ocular surface changes ranging from mild increased tearing or mucus to corneal ulceration and infection. Without correction, some of the resulting ocular changes caused by eyelash deviations can damage vision with permanent scarring and pigmentation or, at worst, corneal perforation and loss of vision.
Definitions
Trichiasis are hairs that originate in a normal location on the skin around the eye but are oriented in an abnormal direction (see below).

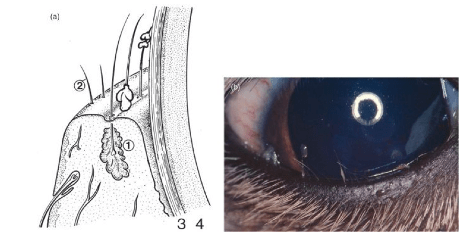
Ectopic cilia are hairs that grow specifically through the conjunctival surface of the inner eyelids and contact the corneal surface, eliciting varying degrees of pain and damage (see below).

Distichiae are hairs that grow in an abnormal location on the eyelid margin (specifically emanating from gland ducts) and are commonly oriented in an inward direction toward the ocular surface (see below).
Trichiasis is everywhere you look, so when is it a problem?
Causes for trichiasis include congenital eyelid agenesis, entropion, ptosis, trichomegaly, and cicatricial eyelid conformation (scarring). Among the three types of eyelash changes discussed in this article, trichiasis tends to be the least prevalent clinically as a clinical problem, but it is associated with more persistent mild to moderate irritation. Dogs with long hair around the eyes, such as Shih Tzus, poodles, terriers, Maltese, Havanese, and bichons, often exhibit varying degrees of trichiasis, which can be more pronounced when other ocular surface issues such as dry eye, nasolacrimal duct congestion, or entropion are also present. For many longer-haired brachycephalic dogs, trichiasis often manifests in conjunction with nasal entropion, which for most is minor and not a true clinical problem in and of itself. In some situations, however, chronic trichiasis will lead to lasting corneal changes, including pigmentation, scarring, and neovascularization. This is often a characteristic of pugs, Pekingese, and Shih Tzus, where varying shades of pigmentation appear in the nasal regions of the cornea, ranging from minor enhanced limbal pigmentation to triangular, whirling scarring to complete clouding over most of the cornea, thereby affecting vision.
Trichiasis can often be found in the nasal or lateral canthus and stem from the medial caruncle (below on the left) or the skin between the nose and the eye (below on the right). Trimming the hairs short may temporarily alleviate the clinical signs in cases with ocular surface irritation or worse (corneal abrasion or ulceration).


x
Others with the same condition, most notably young pugs with advancing corneal pigmentation from the nasal region of the ocular surface, can be treated with medial canthoplasty:

Some breeds, such as Pekingese with chronic facial (nasal) fold trichiasis, will benefit from elective surgery to reduce the size of the folds and increase the distance from the apex of these external skin folds and the ocular surface.

Finally, in older dogs, geriatric ptosis, or upper eyelid drooping, can develop, resulting in previously normal eyelashes constant contact with the ocular surface. With each blink, they trigger surface sensitivity, corneal irritation, and inflammation. For those with notable surface sensitivity, squinting, tearing, ulceration, eyelid modification such as a Stades correction (below) may be beneficial to remove the [geriatric] trichiasis and correct any ptosis or entropion.

Ectopic Cilia are a real threat. What can be done?
While not all cases of trichiasis need correction, every patient who has ectopic cilia should be evaluated with corrective measures in mind. Ectopic cilia can happen in any breed, either solitary or in clusters, which tend to be the most acute and irritating eyelash anomalies. Due to their small size and location, they can also be the most difficult to diagnose. Once identified, complete epilation provides immediate relief and at least temporary reprieve from further irritation, and reduced risk for recurrence in the short term. It is impossible to predict if these hairs will grow back, but it is important that all patients have appropriate follow-up in days to weeks to ensure healing is taking place and the patient is improved. In hard-to-reach or recurrent cilia that continue to irritate, brief general anesthesia may be helpful for dedicated plucking or surgical sharp resection of the offending hairs, including the follicles (see below).

Focal cryosurgery (with proper ocular and skin protection in place) under general anesthesia can also help reduce the risk of regrowth and is typically reserved for more difficult cases. Clinical handheld cautery can also be effectively used to eliminate ectopic cilia but is used with caution because not only could it burn bystander tissue, including the cornea, but cautery may also leave a crusting residue on the conjunctival surface that could contribute to further irritation.
Congenital anomalies, including conjunctival tunnels or pseudo-openings in the palpebral conjunctival surface, can allow ectopic cilia to appear, and many are found within these small circular conjunctival areas that resemble modified conjunctival structures conducive to the presentation or hairs on the conjunctiva (see above). In some breeds, like Shih Tzus, nests of ectopic cilia can be seen beneath the near-transparent conjunctival surface. While they are not breaking through to cause ocular surface irritation, once documented, they should be monitored carefully for eruption through the conjunctival surface and subsequent development of clinical irritation.
Are all Distichiae created equal?
Distichiasis is the most common of all eyelash conditions in practice that produces severe acute or chronic clinical disease. It is important to remember that many dogs go through life with soft distichiae, and it seldom causes any problems. Almost all cocker spaniels, for example, have soft numerous distichia but never have a problem with ocular surface irritation solely due to the hairs alone. Contrast that to a pug, Boston terrier, or bulldog with chronic irritation and corneal scarring from just a few hairs (below). Distichiae arise from normal skin hair follicles that produce hair shafts that utilize the Meibomian or accessory eyelid margin gland openings and follow the path of least resistance onto the eyelid margin. When distichiae are causing corneal damage or are suspected to be the cause of ocular surface pain, they should be removed. Options are manual plucking or surgical removal (more on this later). Distichiae may be rooted or loose, clustered, or single. The distichiae on a poodle will generally be thin, spiraled, and soft, while those found in a French bulldog or boxer will often be straight, stout, and sharp (see below), consistent with the type of hair coat found in the breed.

Distichia can be more problematic in dogs with coexisting eyelid conformation problems, such as English bulldogs, Newfoundlands, Mastiffs, and St. Bernards, where entropion or ectropion can exacerbate the situation. In some of these more complicated patients, multiple surgeries in series may be needed to fully correct the clinical problems (e.g., distichia cryoepilation or plucking followed by entropion repair weeks later). In practice, if a distichia is loose, it may not regrow in the same area. But if it is rooted, then regrowth is expected. Within a given cluster, most hairs will be loose, and the final or last hair to come out is rooted, suggesting a single active follicle is responsible for all the hairs in that cluster. In some breeds and patients, pinning ocular surface irritation on distichiae alone is not always easy. Golden retrievers are one of the breeds where we can see fine, rooted distichia but cannot always tell if it contributes to ocular surface irritation. It is not a bad idea to look for ectopic cilia if distichiae is seen in any clinical patient. It is just to be thorough, as both can be present in any individual with signs of irritation. For plucking any eyelid hairs, veterinarians will use some magnification, often a head loupe or a slit lamp biomicroscope, the best manual restraint possible, topical anesthetic such as proparacaine, calm, steady hands, and an able forceps such as a Jeweler’s forceps (see below).

Do not hesitate to consider sedation and even brief general anesthesia for plucking distichiae in more anxious or fractious pets.
I have plucked, now what?
Supportive care will be important for all types of eyelash conditions. After plucking the offending hairs, careful monitoring will be key to prevent future problems. For ectopic cilia and distichiae, a recheck visit in about four to eight weeks is suggested to monitor for regrowth, sooner if it is suspected there may have been some hairs left behind. The exact timing the hairs can come back is tricky to predict, but if regrowth is seen at the follow-up examinations, then re-plucking or considering a more definitive treatment (surgical removal of the hairs) should be considered if there are ongoing signs of clinical irritation (tearing, discharge, redness, corneal abrasions, etc. Supportive medical care can include topical, non-medicated lubricants (artificial tears) for the non-ulcerated, minimally affected eye. For superficial ulcerated corneas or more significant conjunctivitis and keratitis, consider a short course of topical antibacterials, systemic pain medication, and E-collar as needed. Placement of soft contact bandage lenses on the cornea can also be helpful for some to protect the eye as it recovers, especially if some distichiae are left behind. Dry eye should always be ruled out as a factor for surface irritation, and unfortunately for many brachycephalics, dry eye, and distichia are commonly found together. If keratoconjunctivitis sicca is present, then specific dry eye treatment should be implemented (cyclosporine, etc.).
When is surgery the solution?
When a particular patient keeps returning for the same manual plucking over and over, it may be time to think about surgical removal of the abnormal eyelashes. This is true for all three conditions discussed today. Having said that, some patients and clients are perfectly fine with coming in every couple of months for manual plucking, especially if it is only one or two hairs (often distichia), and the patient is tolerant to the periodic visits and manual restraint needed for this. All eyelash conditions are dynamic, so even after definitive surgery, recurrence is possible. This must be emphasized to all clients. While it only takes one hair to cause significant pain and trauma, in the context of surgery, resolution of eyelash irritation is a numbers game, and all visible, offending hairs should be removed from the area to give the best chance for a good recovery. This holds true especially for distichiae. However, medical management and manual plucking may be the only option if a patient is not a suitable anesthesia candidate.
By far, the most common way we surgically remove distichia is by cryoepilation (see below).

It is a straightforward and highly effective surgery but technically can take a long time, especially if there are multiple distichiae on all eyelids. If the distichiae follicles are frozen and destroyed, no more distichiae can be made. Cryosurgery can be fraught with pitfalls if not done correctly, including skin or eye damage from the liquid nitrogen (corneal shields and towels must be in place), abnormal eyelid scarring, and even eyelid necrosis if done too aggressively, leaving the patient with no eyelid. In rare cases, severe corneal ulceration can complicate recovery and require conjunctival grafting surgery to save the eye. For these reasons, we recommend having this procedure done by a boarded ophthalmologist. Skin depigmentation and minor eyelid margin scarring are common but should not affect eyelid functionality, and the effects of the freezing are more severe in smaller breeds with thinner eyelids. Alternatively, sharp excision may be appropriate for one or two hairs, ensuring that complete follicle resection is achieved and eyelid margin confluence is preserved.
Playing the long game with T.E.D.
Hopefully, this information provided a better understanding of the distinction and clinical approaches to the more common eyelash issues in dogs. Just remember T.E.D.: trichiasis, ectopic cilia, and distichia. While distichiasis is the more common clinically relevant problem seen in clinical practice, all types can lead to serious discomfort–even vision loss–without proper recognition and treatment. Ectopic cilia and distichaie have more potential to cause acute pain and more significant corneal damage. Trichiasis (especially nasal trichiasis) may be the most common observed condition of the three, but it is not always a clinical problem.
The options for treatment for all eyelash problems are variable and may range from a simple one-time pluck to more extensive surgery. In all scenarios, the follow-up is never truly complete, as the specter of recurrence is always there. Fortunately, for most cases with the right approach, there is a point when a) the patient is finally better, b) monitoring and visits become infrequent, and c) the condition does not return.
In conclusion, the distinct types of eyelash problems are illustrated below:

Courtesy of the PDSA website: https://www.pdsa.org.uk/pet-help-and-advice/pet-health-hub/conditions/eyelash-problems-in-dogs
x
Reference
Gelatt, Kirk N. and Gilger, Brian C. Veterinary Ophthalmology: Two Volume Set.