-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Referrals
- Referral Forms/Contact
- Direct Connect
- Referring Veterinarian Portal
- Clinical Articles
- Partners in Care Newsletter
CE, Internships & Alumni Info
CE Seminar Schedule
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 By Kiko Bracker, DVM, DACVECC
By Kiko Bracker, DVM, DACVECC![]()
angell.org/emergency
emergency@angell.org
617-522-7282
March 2022
Feline hyperaldosteronism is likely the most common adrenocortical disease affecting cats. It is rarely identified in dogs, with only a few sporadic case reports testifying its existence in that species. The eponym Conn’s syndrome is sometimes applied to primary hyperaldosteronism after Jerome Conn, who first identified the issue in humans in 1955.1 Tumors of the adrenal cortex or adrenal cortical hyperplasia can cause excessive aldosterone secretion. Aldosterone is a hormone that balances sodium and potassium levels. It results in sodium being resorbed in the distal convoluted tubule of the loop of Henle and potassium being excreted into the urine in the collecting ducts of the distal nephron.
adrenocortical disease affecting cats. It is rarely identified in dogs, with only a few sporadic case reports testifying its existence in that species. The eponym Conn’s syndrome is sometimes applied to primary hyperaldosteronism after Jerome Conn, who first identified the issue in humans in 1955.1 Tumors of the adrenal cortex or adrenal cortical hyperplasia can cause excessive aldosterone secretion. Aldosterone is a hormone that balances sodium and potassium levels. It results in sodium being resorbed in the distal convoluted tubule of the loop of Henle and potassium being excreted into the urine in the collecting ducts of the distal nephron.
Hyperaldosteronism can be tricky to identify because it is not high on our radar of feline illnesses. It results in a fairly predictable collection of clinical and clinicopathological abnormalities that can strongly suggest hyperaldosteronism as the cause of illness when viewed together.
Profound hypokalemia (<3.0mEq/L) is often the first abnormality identified that triggers suspicion of hyperaldosteronism. Low potassium is seen in 90% of cats with this problem. Interestingly, hypernatremia is not commonly seen since it is usually balanced by water resorbed with excess sodium. Other clin path irregularities include mild azotemia (50% of cases), creatine kinase (CK) elevation (95% of cases), and an elevated aldosterone level is seen in about 90% of cases.2, 3 A serum potassium level of <3.0mEq/L on initial lab work in a patient not taking furosemide is almost always due to either potassium wasting from chronic kidney disease or hyperaldosteronism in our experience.
 The clinical or historical signs of hyperaldosteronism are relatively non-specific. These patients generally present with lethargy, weight loss, and historical PU/PD. But if a patient also shows ventral neck flexion due to low potassium or hypertension, which can result in intraocular hemorrhage or retinal detachment – the leap to suspicion of excessive aldosterone secretion is made more easily.
The clinical or historical signs of hyperaldosteronism are relatively non-specific. These patients generally present with lethargy, weight loss, and historical PU/PD. But if a patient also shows ventral neck flexion due to low potassium or hypertension, which can result in intraocular hemorrhage or retinal detachment – the leap to suspicion of excessive aldosterone secretion is made more easily.
The next diagnostic steps will likely be an abdominal ultrasound and an aldosterone level. But a serum potassium level of <3.0mEq/L often warrants some intervention before those two tests can be accomplished. If the potassium level nears 2.0mEq/L, respiratory muscle weakness and hypoventilation can result.5, 6 Profoundly weak or azotemic hypokalemic cats should be hospitalized for IV fluid therapy and aggressive IV potassium supplementation. More stable patients can be supplemented with oral potassium gluconate at 2-6mEq/cat BID.3, 4
Aldosterone secretion is directly related to the blood potassium level. Aldosterone’s primary action is to reduce/excrete potassium. If the blood potassium level is low, then aldosterone secretion should be maximally shut off in the normal patient. Even a hypokalemic patient’s aldosterone level within the normal range would be considered too high and suggestive of aldosterone hypersecretion. An aldosterone level should be submitted before supplementation with potassium if at all possible. Either a spun and separated EDTA plasma sample or a clot tube can be used to evaluate an aldosterone level with a minimal sample requirement of 0.5-1.0ml of plasma or serum. The turnaround time can be up to a week, so prompt submission of this sample is helpful. Consult your lab about specific sample and shipping requirements.
Abdominal ultrasound is the most commonly used imaging modality to identify the source of suspected aldosterone secretion. Single adrenal tumors are the most common finding, often with a small to normal contralateral adrenal gland. Adrenal cortical hyperplasia may manifest itself as bilateral adrenal enlargement. Bilateral adrenal adenomas have even been identified.3 Invasion of the vena cava is uncommon in only about 10% of cases. Caval involvement is more critically evaluated with an abdominal CT scan.2
Cats with concurrent diabetes mellitus or a Cushingoid appearance may also have excessive adrenocortical progesterone secretion. Excessive progesterone has an anti-insulin effect and can be the driving force for the development of diabetes. Progesterone also suppresses the Hypothalamic-Pituitary-Adrenal axis and results in low cortisol secretion. ACTH stimulation tests on these cats may help identify inadequate cortisol secretion. On ultrasound or CT, an atrophic in the inapparent contralateral adrenal gland may suggest adrenocortical insufficiency once the affected adrenal gland is removed. The post-operative management may need to include a tapering dose of steroid and mineralocorticoid to avoid a (mild) Addisonian crisis. Concurrent progesterone secretion/cortisol insufficiency/diabetes mellitus is more commonly seen with adrenocortical carcinomas. Diabetes mellitus can go into remission several months after the affected adrenal gland is removed.9 These cats should be rechecked within 1-2 weeks of surgery to assess for biochemical evidence of adrenocortical insufficiency (chemistry panel, +/- ACTH stim test).
Medical treatment should be started once a diagnosis is made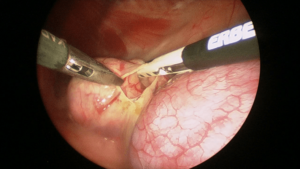 or is confidently suspected. The bilateral adrenal disease must be managed medically (no surgical option), and cats with unilateral disease who are contemplating surgical adrenalectomy should be stabilized medically for several weeks before surgery. It can be tough to achieve an adequate potassium level with potassium supplementation alone on an outpatient basis.2, 3 Spironolactone, an aldosterone antagonist and mild diuretic, at 1-2mg/kg BID should be used in conjunction with potassium supplementation.3, 4Although spironolactone has some mild diuretic effect, it is not potent enough to cause the mildly azotemic cat to worsen at home. However, a subcutaneous fluid can easily be added at home to avoid this potential complication. Even when using spironolactone and potassium gluconate together, a normal potassium level is usually difficult to achieve – but normal should not be the goal. Try to keep the serum potassium level 3.0-4.0mEq/L, which is usually enough to avoid any complications of hypokalemia. Hypertension (>160mmHg) is best treated with amlodipine at 0.625-1.25mg/cat SID-BID.7 If retinal detachment is present, then BID dosing should be considered to control hypertension quickly and maximize the possibility of retinal reattachment.
or is confidently suspected. The bilateral adrenal disease must be managed medically (no surgical option), and cats with unilateral disease who are contemplating surgical adrenalectomy should be stabilized medically for several weeks before surgery. It can be tough to achieve an adequate potassium level with potassium supplementation alone on an outpatient basis.2, 3 Spironolactone, an aldosterone antagonist and mild diuretic, at 1-2mg/kg BID should be used in conjunction with potassium supplementation.3, 4Although spironolactone has some mild diuretic effect, it is not potent enough to cause the mildly azotemic cat to worsen at home. However, a subcutaneous fluid can easily be added at home to avoid this potential complication. Even when using spironolactone and potassium gluconate together, a normal potassium level is usually difficult to achieve – but normal should not be the goal. Try to keep the serum potassium level 3.0-4.0mEq/L, which is usually enough to avoid any complications of hypokalemia. Hypertension (>160mmHg) is best treated with amlodipine at 0.625-1.25mg/cat SID-BID.7 If retinal detachment is present, then BID dosing should be considered to control hypertension quickly and maximize the possibility of retinal reattachment.
The prognosis with medical management alone is very good, and survival times can be measured in years.3 Cats on medical management will need to remain on medication lifelong and have occasional BP and renal panel assessment. It is common for azotemia to gradually worsen over months to years due to imperfect control of hypertension and the profibrotic effects of aldosterone, which further damages the kidneys.
Surgical management is often the treatment of choice if a unilateral adrenal mass or enlargement is identified. Left adrenal tumors are easier to access than right-sided masses since the right kidney and adrenal gland are tucked up in the liver’s renal fossa, making access challenging. Once the affected adrenal gland is removed, prior hypertension and hypokalemia resolve relatively quickly, and no further medication is needed. The benefit of surgery for a unilateral adrenal disease is that medications can be stopped, and the gradually detrimental renal effects of excess aldosterone secretion can be avoided. After adrenalectomy, survival times for an adrenal cortical adenoma or an adrenal carcinoma were not significantly different, with a combined median survival time of 1,297 days.2 Carcinomas and adenomas are identified with about the same frequency.2, 3
References
- JW Conn. Primary Aldosteronism. J Lab Clin Med 1955;45:661-664.
- AJ Lo, et al. Treatment of aldosterone-secreting adrenocortical tumors in cats by unilateral adrenalectomy: 10 cases (2002-1012). J Vet Intern Med 2014;28:137-143.
- RA Ash, A Harvey, S Tasker. Primary hyperaldosteronism in the cat: a series of 13 cases. J Fel Med Surg 2005;7:173-182.
- S Djajadiningrat-Laanen, S Galac, H Kooistra. Primary hyperaldosteronism – expanding the diagnostic net. J Fel Med Surg 2011;13:641-650.
- TN Hammond, JL Holm. Successful use of short-term mechanical ventilation to manage respiratory failure secondary to profound hypokalemia in a cat with hyperaldosteronism. J Vet Emerg Crit Care 2008;18(5):517-525
- S Haldane, et al. Profound Hypokalemia Causing Respiratory Failure in a Cat with Hyperaldosteronism. J Vet Emerg Crit Care 2007;17(2):202-207.
- J Bisignano, DS Bruyette. Feline hyperaldosteronism: treatment and prognosis 2012. Vet Med;107(3):118-125.
- J Bisignano, DS Bruyette. Feline hyperaldosteronism: recognition and diagnosis 2012. Vet Med;107(3):118-125.
- C Harro, et al. Retrospective study of aldosterone and progesterone secreting adrenal tumors in 10 cats. J Vet Intern Med. September 2021;35(5):2159-2166.