-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Referrals
- Referral Forms/Contact
- Direct Connect
- Referring Veterinarian Portal
- Clinical Articles
- Partners in Care Newsletter
CE, Internships & Alumni Info
CE Seminar Schedule
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 By Shawn Kearns, DVM, DACVIM
By Shawn Kearns, DVM, DACVIM
angell.org/internalmedicine
internalmedicine@angell.org
617-541-5186
Hypersomatotropism (HST) is characterized by excess production and secretion of growth hormone (GH) while acromegaly is the clinical syndrome that develops as a result of the excess growth hormone. Feline hypersomatropism is most commonly caused by a growth-hormone producing pituitary gland adenoma.
Clinical signs are often slow to develop and are not present in all cats with hypersomatotropism at the time of diagnosis. The average age at presentation is ~10-11 years and males are more commonly affected. Most patients have diabetes mellitus at the time of diagnosis due to the diabetogenic effects of growth hormone, but resistance may not be present until later in the disease course. Hyperglycemia will lead to typical signs of polyuria and polydipsia while signs of polyphagia may be due to the hyperglycemia or effects of excess GH. Despite unregulated diabetes, many patients will have a normal to increased body weight and condition score. HST has been diagnosed prior to the development of diabetes and in those reported cases, clinical signs at presentation included a range of neurologic signs, plantigrade/palmigrade stance and weight gain despite no change in diet. 1
Due to the growth promoting effects of growth hormone and insulin-like growth factor 1 (IGF-1), other clinical signs may include increased paw size, broad facial features, prognathia inferior, increased inter-dental space and a large tongue. The difference between patients with HST and unaffected may be small, though, making recognition of feline acromegaly-based facial features alone insensitive.2 Other exam findings may include a heart murmur and palpable organomegaly. Cardiac and other organ changes are common due to the effects of growth hormone. A recent study reviewed ultrasound findings in patients with acromegaly versus age matched controls and found that acromegalic patients often have measurably larger kidneys, adrenal glands and increased pancreatic thickness. If these findings are noted on ultrasound, even without the presence of diabetes, acromegaly should be considered.3 Likewise, many cats will also have echocardiographic abnormalities including left ventricular concentric hypertrophy, left atrial enlargement and diastolic dysfunction.4
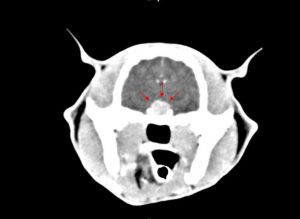
A tentative diagnosis is based on documentation of an increased serum IGF-1 concentration. IGF-1 is a useful screening parameter due to the fact that it reflects 24-hour GH secretion, parallels changes in GH, is not pulsatile in nature (unlike GH) and is a sensitive marker for GH excess. An IGF-1 > 1000ng/ml (131nmol/L) is generally accepted as strongly suggestive of HST. Recently an enzyme linked assay for IGF-1 was validated in cats and was found to have a sensitivity of 100% and specificity of 88% at a cut-off of 997ng/ml.5 If levels are 800-1000ng/ml, retesting is recommended. This cutoff may result in underestimation of the true prevalence due to potential lower levels in early or mild forms of the disease. In newly diagnosed diabetics, it is recommended to test only after 6-8 weeks of insulin therapy. The reason for this is that hepatic IGF-1 production is dependent on insulin in the portal circulation. Ideally, the presence of a pituitary mass would be confirmed with computed tomography (CT) or magnetic resonance imaging (MRI), however, a small number of cases may not show pituitary enlargement.
According to a recent report, the prevalence of acromegaly may be underestimated. In a total of 1221 cats, 319 patients had IGF-1 levels > 1000ng/ml and of those patients with follow-up imaging, pituitary lesions were confirmed in 56 (89%). This study confirmed a positive predictive value of 95% using IGF-1, but also highlighted the need to test appropriate patients.6
Treatment can be conservative or more targeted in nature. The conservative approach involves management of the diabetes mellitus; this treatment should be reserved for cases in which definitive treatment is not available or is declined by owners. The high doses of insulin needed to control these patients may also be cost prohibitive as some patients require TID-QID dosing of a long-acting insulin such as glargine or detemir. 
Transsphenoidal hypophesectomy has been reported for the treatment of feline acromegaly and can lead to complete remission of neurologic and diabetic signs.7 This procedure, however, has limited availability and requires an experienced neurosurgeon. In addition, surgery often results in compete removal of the pituitary gland so patients often require supplementation post-surgery with steroids, l-thyroxine and desmopressin. Subsequently, only patients that are easy to medicate should be considered for this procedure.
Single fraction modified radiosurgery was shown to be successful in improving clinical signs in the majority of patients, including improved insulin response and neurologic signs. In 11 cats evaluated, the median survival time was 25 months (1-60 months).8 Hypo-fractionated radiotherapy was also evaluated retrospectively in 14 cats. In this study, 13/14 had improved glycemic control that was sustained for up to 60 months, however 2 eventually did have progressive disease and one failed to respond.9 Due to the need for repeated anesthesia, patients with cardiac or renal disease may be at increased risk for this therapy. Response times are variable, and though many patients have improvement in glycemic control, insulin is often still required.
Recently pasireotide was evaluated for the medical management of HST in feline patients. Pasireotide is a novel multi-receptor ligand somatostatin analog that has been shown to improve biochemical control of human patients with HST. Somatostatins act on the pituitary gland to inhibit growth hormone release. In addition, they can act peripherally by interfering with GH receptor binding on hepatocytes and may induce apoptosis in pituitary adenomas resulting in shrinkage. The drug is given SQ every 12-24 hours or can be administered monthly with a long-acting formulation. In this study, IGF-1 levels decreased significantly with treatment and this decrease was associated with increased insulin sensitivity.10 The main adverse effects reported were gastrointestinal upset including soft voluminous stools and gas-distended intestines. Cost remains a limiting factor in the use of this drug.
HST is an under-recognized disease in our feline patients. Testing should be considered in those patients with difficult-to-regulate diabetes, organomegaly of unknown cause, unexplained weight gain or changes in facial/body features as well as neurologic signs. Patients that respond well to surgery, radiosurgery or radiotherapy can have improved glycemic control and survival with a good quality of life.
References
- Fletcher JM, Scudder CJ et al. Hypersomatotropism in 3 cats without concurrent diabetes mellitus. J Vet Intern Med 2016; 30 (4): 1216-21
- Lamb CR, Ciasca TC et al. Computed tomography signs of acromegaly in 68 diabetic cats with hypersomatotropism. J Feline Med Surg 2014; 16 (2): 99-108
- Lourenco BN, Randall E et al. Abdominal ultrasonographic findings in acromegalic cats. J Feline Med Surg 2015; 17 (8): 698-703.
- Myers JA, Lunn KF, Bright JM. Echocardiographic findings in 11 cats with acromegaly. J Vet Intern Med 2014; 28 (4): 1235-1238
- Rosca M, Forcada Y et al. Screening diabetic cats for hypersomatotropism: performance of an enzyme-linked immunosorbent assay for insulin- like growth factor 1. J Feline Med Surg 2014; 16 (2): 82-8
- Niessen JM, Forcada Y et al. Studying cat (felis catus) diabetes: beware of the acromegalic imposter. PLoS One 2015; 10 (5): e0127794
- Meij BP, Auriemma E et al. Successful treatment of acromegaly in a diabetic cat with transsphenoidal hypophysectomy. J Feline Med Surg 2010; 12 (5): 406-10
- Sellon RK, Fidel J et al. Linear accelerator based modified radiosurgical treatment of pituitary tumors in cats: 11 cases (1997-2008).
- Dunning MD, Lowrie CS et al. Exogenous insulin treatment after hypofractionated radiotherapy in cats with diabetes mellitus and acromegaly. J Vet Intern Med 2009; 23 (2): 243-9
- Scudder CJ, Gostelow R et al. Pasireotide for the medical management of feline hypersomatotropism. J Vet Intern Med 2015; 29 (4): 1074-80.