-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Referrals
- Referral Forms/Contact
- Direct Connect
- Referring Veterinarian Portal
- Clinical Articles
- Partners in Care Newsletter
CE, Internships & Alumni Info
CE Seminar Schedule
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 By Martin Coster, DVM, MS, DACVO
By Martin Coster, DVM, MS, DACVO![]()
angell.org/eyes
ophthalmology@angell.org
617-541-5095
June 2023
x
x
Iris hyperpigmentation is commonly encountered in cats, but clinical management of these cases is challenging since the pigment can represent anything from benign change (melanosis) to malignant neoplasia (feline diffuse iris melanoma, FDIM, Figure 1).

Figure 1: Histopathologically-confirmed feline diffuse iris melanoma, of the cat’s right eye, in contrast to the normal yellow iris coloration of the left eye.
Iris melanosis is a benign increase in melanocytes on the surface of the iris. Feline diffuse iris melanoma is a malignant clonal expansion of these melanocytes in an uncontrolled and disorganized fashion. It is presumed that iris melanoma can develop from iris melanosis, but the process is very unpredictable. The terminology of “diffuse” iris melanoma may also be misleading since some melanoma can be focal on the iris surface.
The veterinary literature is relatively sparse for peer-reviewed research on the topic. A 2016 survey1 of board-certified veterinary ophthalmologists, in which case details and photos were presented, and the ophthalmologist was asked to make a diagnosis of melanosis or melanoma, showed that even experienced clinicians have a difficult time determining the significance of iris hyperpigmentation, even when expressing confidence in their opinion. Factors that enhanced correct identification were lesion thickness, progression over time, surface area of involvement, pupillary light reflex testing, intraocular pressure, and the presence of uveitis (aqueous flare). In this authors’ experience, the most challenging diagnoses are the intermediate cases lying somewhere on the spectrum between small foci and complete iris surface pigmentation.
Given this caveat, Figures 2 to 4 show three hyperpigmented lesions in three cats. The examiner’s opinion was that each was an example of iris melanosis. Key determinants of these opinions included the following:
- The lack of raised/thickened tissue. Generally, the mitotic activity of melanoma will lead to the thickening of the layer of pigment, whereas melanosis is from an accumulation of normal melanocytes in their normal location.
- Heterogeneity of the lesion on microscopic examination. Iris melanoma often develops a more homogeneous “velvet-like” appearance due to the clonal expansion of pigmented cells with little structural detail of the normal iris remaining.
- Lighter pigment due to a lower melanin component in the pigmented cells.
- Normal iris excursions during pupillary light reflexes (PLR). Iris melanoma may invade deeper into the iris stroma than iris melanosis, affecting the pupillary muscles.
- Normal intraocular pressure, absence of any uveitis or glaucoma.
- Absence of pigment dispersion elsewhere within the anterior chamber (e.g., pigment on the lens capsule, corneal endothelium, or free-floating in the aqueous humor).
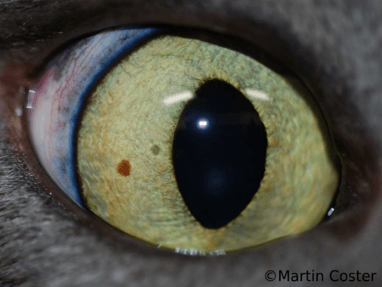
Figure 2: Focal hyperpigmented lesion in the lateral iris of the right eye of a cat. This may be described as an iris freckle.
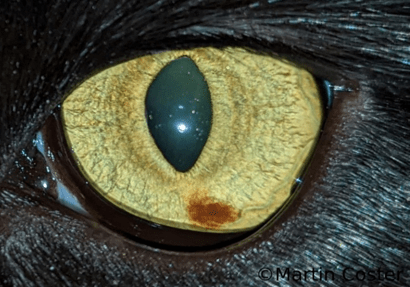
Figure 3: Focal hyperpigmented lesion in the inferior iris of the left eye of a cat. A larger freckle may be described as a nevus.

Figure 4: Focal hyperpigmented lesion in the inferior-medial iris of the right eye of a cat.
Nevertheless, any hyperpigmented iris lesion should be monitored with time. The owners should be educated that the “diagnosis” is often, at best, a clinical suspicion and that growth of the lesion or conversion to iris melanoma may occur at any time.
Iris biopsy2 may be offered by a veterinary ophthalmologist to provide a more precise diagnosis. Under general anesthesia, two small limbal incisions are made, the anterior chamber is filled with a viscoelastic agent to maintain its form, and the iris lesion is grasped with forceps and biopsied with iris scissors. The viscoelastic agent is then removed, and the limbal incisions are sutured. Complications can include hemorrhage, uveitis, pupil abnormalities, and corneal ulceration. Importantly, there is no guarantee that the lesion will be appropriately sampled, with melanoma being possibly misidentified as melanosis or not identified at all. For more scattered or diffuse lesions (e.g., Figure 5), the area sampled will be critical to achieving the correct diagnosis.
With advancing age, iris melanosis may become more diffuse, often appearing in a “tiger-stripe” formation (Figure 5). Possibly, pupillary excursions provide pressure that aligns the melanocytes. These eyes should be closely monitored for darker or raised areas of pigment developing or any interruption of the pupillary excursions during the PLR.

Figure 5: Relatively generalized iris hyperpigmentation of the right eye of a cat. Although this is clinically suspected to be a variant of iris melanosis, histopathology is needed to rule out feline diffuse iris.
Further darkening and coalescing of the hyperpigmented areas may lead to an iris like that of Figure 6. At this point, knowing a definitive diagnosis based on clinical examination alone is impossible. While much of the pigment may remain flat, lighter in coloration, and heterogeneously dispersed, there may be darker, thicker, more homogeneous areas consistent with focal melanoma in a background of melanosis. The presence of uveitis, glaucoma, pigment dispersion, and/or disturbance of PLR would be more indicative of FDIM.

Figure 6: Relatively generalized iris hyperpigmentation of the right eye of a cat. It is impossible to determine if this is iris melanosis or feline diffuse iris melanoma without an accurate biopsy for histopathology.
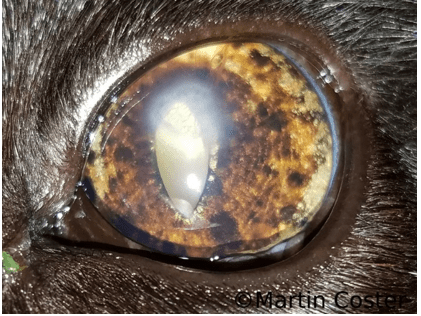
Figure 7: Feline diffuse iris melanoma, confirmed with histopathology, in the left eye of a cat. The hazy area is a vascularized corneal ulcer or associated scar tissue.
Figure 7 shows further progression of iris hyperpigmentation, with an extremely high index of suspicion for FDIM. The pigmented areas are darker, with some raised with a homogeneous velvety appearance; this case was confirmed as FDIM with histopathology following enucleation.
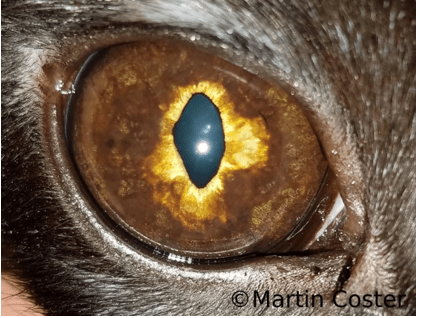
Figure 8: Feline diffuse iris melanoma, confirmed with histopathology, in the right eye of a cat.
Figure 8 shows profound thickening of the iris pigment, with a more homogeneous velvety appearance and distortion of the pupillary margin, a definitive FDIM.
If FDIM is suspected, the author recommends a full metastasis screening, including bloodwork, thoracic radiographs or thoracic computed tomography (CT), and abdominal ultrasound or CT. Sites of melanoma metastasis can include but are not limited to local lymph nodes, lungs, liver, spleen, kidneys, and rarely the contralateral eye. However, it must be cautioned that early metastatic lesions may be missed even with extensive and advanced diagnostics.
A landmark 2002 paper examined survival times in enucleated cats with confirmed FDIM compared to control cats, concluding that “early enucleation is important to avoid premature death, presumed to be due to cancer metastasis in cats with diffuse iris melanoma.”3 Importantly, cats with glaucoma secondary to FDIM appeared to have a lower survival rate of 21% (four of 19) compared with 73% (11 of 15) of cats without glaucoma (although the difference only approached statistical significance). This was likely because glaucoma develops secondary to a more extensive invasion of the melanoma into the ocular tissues and associated uveitis/inflammation from the destructive tumor. However, a more recent 2016 study4 did not show an increased risk of metastasis in cats with glaucoma, suggesting both that metastasis can occur before glaucoma develops and that glaucoma itself does not increase the metastasis rate. This study still recommended the enucleation of glaucomatous eyes with FDIM.
If hyperpigmented lesions are detected early, close monitoring should be initiated every two to three months, including photodocumentation and intraocular pressure. Transcorneal diode laser treatment has been described5 as a way to limit the progression and spread of focal lesions and even to treat diffuse iris hyperpigmentation (whether melanosis or melanoma) to halt the progression to or of melanoma. The cat is anesthetized in this procedure, and diode laser energy is applied through the cornea until the pigmented regions shrink by 50% or more. Although distortion of the pupillary margin and associated post-operative light sensitivity is a likely outcome, corneal ulceration, hyphema, and/or uveitis may occur as secondary complications, the procedure is generally considered safe. Results are variable, and it is a matter of continued debate whether pigment progression is halted or only temporarily slowed (Figures 9 and 10).
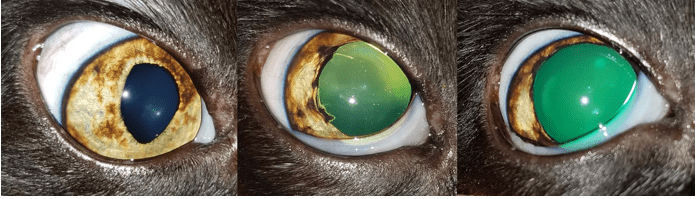
Figure 9: Iris hyperpigmentation in the right eye of a cat before lasering (left), and the appearance 11 days (middle) and four months (right) following transcorneal diode laser. See Figure 10 for further follow-up.
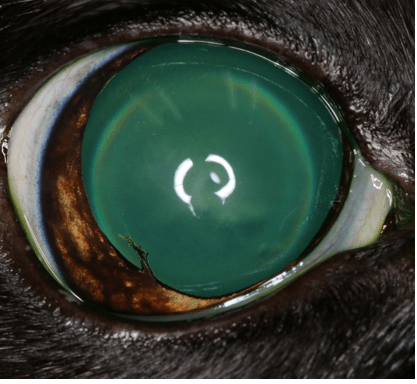
Figure 10: Three-and-a-half-year follow-up of the eye in Figure 9, showing the progression of iris hyperpigmentation (and focal posterior synechia from prior laser therapy). Enucleation confirmed feline diffuse iris melanoma. The cat was staged, and melanoma was not found elsewhere. It is unknown whether the initial laser procedure slowed lesion progression or lowered metastasis risk. Photo courtesy of Tanja Nuhsbaum DACVO.
Possibly the biggest quandary in managing feline iris hyperpigmentation is deciding when to enucleate a progressively pigmenting eye. Factors such as the cat’s age, comorbidities, the health of the other eye, and the owner’s risk tolerance must be weighed. The opinions of veterinary ophthalmologists vary widely. This author has seen metastatic disease and orbital melanoma (“localized recurrence”) develop several years following enucleation. The author, therefore, counsels laser treatment for small progressive lesions and early enucleation for more generalized progressive disease.
Once, and only once, the primary disease has been removed via enucleation and a diagnosis of FDIM confirmed, the author offers the owner referral to an oncologist for a melanoma vaccine series. The melanoma vaccine, Oncept,6 is a USDA-licensed therapeutic vaccine proven to extend the lives of dogs treated for oral melanoma. Its use in cats for follow-up after iris melanoma surgery is considered off-label; it is not licensed nor formally approved for use in this species for this disease.
In one study, published in 2015 in the Journal of Feline Medicine and Surgery,7 studied 24 cats with malignant melanoma of various types (only found with ocular or periocular melanoma) that were administered the vaccine. It was concluded that the canine melanoma vaccine can be safely administered to cats with minimal risk of adverse effects. Seven of the 24 cats experienced a mild adverse effect of the vaccine (11% of the total number of 114 vaccinations given), which included pain on vaccine administration, brief muscle irritation, transient inappetence, depression, nausea, and a mild increase in pigmentation at the injection site. Unfortunately, 14 of the 24 cats went on to succumb to melanoma. The vaccine’s efficacy could not be assessed in this paper, and a third of the cats already had known metastasis, which is a different population from those typically enucleated for FDIM. Given that the vaccine is safe and may prevent the development of metastatic melanoma or delay its onset, some cat owners choose to complete the vaccination series and return for boosters.
Author’s Disclaimer
Given the relative paucity of peer-reviewed literature and ongoing debate in the veterinary ophthalmology profession about best practices in diagnosing and managing feline iris hyperpigmentation, many of the statements in this article are derived from the author’s own clinical experience.
x
References
- Amissah et al. (2022). Prevalence and characteristics of cannabis-induced toxicosis in pets: Results from a survey of veterinarians in North America. PLOS ONE, 17, 1–18
- Brutlag, A., & Hommerding, H. (2018). Toxicology of marijuana, synthetic cannabinoids, and cannabidiol in dogs and cats. Veterinary Clinics: Small Animal Practice; 48, 1087–1102.
- Fitzgerald et al. (2021). Detecting and quantifying marijuana metabolites in serum and urine of 19 dogs affected by marijuana toxicity. Journal of Veterinary Diagnostic Investigation, 33:1002–1007.
- Gwaltney-Brant, S. & Meadows, I. (2018). Intravenous lipid emulsions in veterinary clinical toxicology. Veterinary Clinics: Small Animal Practice, 48, 933–942.
- Meola et al. Evaluation of trends in marijuana toxicosis in dogs living in a state with legalized medical marijuana: 125 dogs (2005–2010). JVECC 2012; 22, 690–696
- Robben, J.H., & Dijkman, M.A. (2017). Lipid therapy for intoxications. Veterinary Clinics of North America: Small Animal Practice; 47, 435-450.