-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 By Michael Pavletic, DVM, DACVS
By Michael Pavletic, DVM, DACVS
Director of Surgical Services
angell.org/surgery
617-541-5048
Historically, a variety of topical agents have been used in managing open wounds, and the list of these products is rather long. Today there are dozens of topical agents and dressings marketed for wound care, mostly for human patients. Unfortunately, the true efficacy of all current topical products cannot be accurately assessed without well-designed comparative studies. An excellent reference regarding wound care products is Thomas’ Surgical Dressings in Wound Management (See reference.) Most pharmaceutical research includes the use of rats, rabbits, and pigs. Although clinical applicability of studies between species is open to debate, research results can serve as general guidelines regarding the use of wound care products in veterinary patients.
There is a renewed interest in natural wound care products, both in human and veterinary medicine. A natural product by definition is any compound or substance found in nature or in a broader sense, natural products include any substance produced by life. Many of the topical products noted can be considered “natural,” including chitosan, collagen, alginates, etc. As a natural product, honey and sugar are readily available for use in wound care. This article is devoted both to the medical science and clinical use of these two natural products.
Honey
Honey has a broad history in its use in wounds. There are numerous historical references of its use in early Sumerian clay tablets (4,000 years ago); ancient Egypt (1700 BC); ancient Chinese medicine; Native Americans; ancient Greeks; and East African tribes. Honey is essentially a super-saturated solution comprised of sugars (38.2 % fructose, 31% glucose, 7.35% maltose, 1.3% sucrose— on average) with small amounts of amino acids (50% being proline), minerals, organic acids, vitamins, enzymes. However, the composition of honey does vary according to the geographical source.
Of interest are the enzymes contained in honey, including: invertase (converts sucrose to glucose and fructose); amylase (breaks down starch); glucose oxidase (converts glucose to hydrogen peroxide); and gluconolactone (forms gluconic acid); catalase (converts peroxide to glucose oxidase, oxygen and water); and acid phosphatase (separates inorganic phosphates from organic phosphate). The low pH (3.5-6.0) of honey is the result of the multiple organic acids present.
The antibacterial activity of honey is the results of several factors (called inhibins). Hydrogen peroxide (produced by glucose oxidase) is produced when diluted with water. Content varies with various honey. A second antibacterial component is found in honey produced from the flowers of the New Zealand Manuka bush (Leptospermum scoparium). [Jelly Bush is honey obtained from Australia (Leptospermum sp.)] The antibacterial properties of this honey “Unique Manuka Factor” or UMF varies in batches of honey.
The antibacterial properties of the UMF can be rated by measuring its equivalency to dilutions of phenol (carbolic acid). In other words, the relative UMF antibacterial activity of a given source of Manuka honey is rated by its relative equivalency to the comparable antibacterial activity of a corresponding concentration of a given phenol dilution. A classification of relative UMF concentration was developed: for medical applications a basic rating of 10 was proposed although some batches of Manuka honey can rise to a rating of 25. Unfortunately, this rating system can be misrepresented. It has been proposed that medical grade Manuka honey should have a “non-peroxide” equivalency of a 12% Phenolic concentration. New Zealand Manuka honey can have a wide range of potency from <2% to 58% phenolic antibacterial activity.
It has been proposed that the Unique Manuka Factor (UMF) may be in part due to the compound methylglyoxal (MGO): an MGO concentration of 100mg/kg is required in honey used for medical applications. Unfortunately, the MGO rating system is not considered accurate: MGO concentration and antibacterial activity are not linear. For example, doubling the MGO concentration does not result in a similar rise in the UMF value. Flavenoids and plant-derived phenolics also may be responsible for the honey’s antibacterial properties.
Besides the antibacterial properties of honey containing peroxide, and the non-peroxide UMF factor, the high acidity of honey (pH 3.5 to 6.0) also has antibacterial properties. Honey has been demonstrated to be useful in treating the biofilm of infected wounds, neutralizing destructive free radicals in chronic wounds, and promoting the healing processes. Wound-healing attributes reported for honey include stimulation of macrophage migration, angiogenesis, fibroplasia, and epithelialization.
Raw honey may also contain bacterial and fungal contaminants, including anaerobic spore-forming organisms. It is for this reason that medical honey in all its forms must be sterilized for human use, despite the fact that the relative risk of infection is considered low. Based on the considerable research that demonstrates the benefits of this natural product, veterinarians should take a more serious look at the use of medicinal honey in wound management. [It must be noted that most commercial honey purchased in grocery stores has been highly refined: as a result, its anti-bacterial effect is likely due to the high sugar content.]
Both honey and sugar are hygroscopic agents with a high osmolarity that have been used to reduce local tissue edema. This hyperosmolarity also can inhibit or kill bacteria while promoting granulation tissue. The high sugar content may provide an alternate source of energy both to the viable tissues and bacteria. Bacteria may use glucose over the amino acids present in the wound and may, in turn, produce lactic acid rather than malodorous discharge from the putrefaction of the nonviable tissue proteins.
Sugar
Unlike the beneficial antibacterial properties noted in honey, sugar primarily reduces bacterial proliferation due to its high osmolarity, thereby reducing moisture content in the wound. Sugar also is reported to enhance macrophage migration, granulation, tissue formation, and epithelialization. Various “over the counter” sugar products are not sterile. Powdered sugars also contain calcium phosphate or sodium aluminum silicate to prevent caking during storage. Powdered sugars can be used to form a topical paste to apply to open wounds (see below).
Clinical Application of Honey and Sugar
In human wound care, use of honey dressings (sterilized by ionizing radiation) is the common method of applying honey to a wound. Large areas of necrotic tissue are best surgically debrided prior to application of honey or sugar. Both should be applied liberally to the wound, followed by the application of a dressing and a thick outer absorptive layer to help retain discharge from the wound surface. Bandage changes may be initially performed daily and altered according to the clinician’s assessment of the wound. Wounds may be lavaged with sterile saline and inspected prior to their reapplication. Gauze also can be soaked in honey to simplify its application to the wound, keeping in mind the gauze may adhere to viable tissues and cause pain and irritation during its removal.
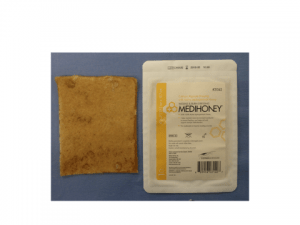
Figure 1: Medihoney Dressing. (From Pavletic MM. (2018). Atlas of Small Animal Wound Management and Reconstructive Surgery, 4th Edition. Ames, Iowa: Wiley-Blackwell.)
Sugar can be poured into the wound with a 1-cm plus layer over the wound surface, followed by a topical dressing and bandage wrap. Bandage changes also may be performed daily and modified according to the wound’s condition. Because granulated sugar has a tendency to spill, isolating (“corralling”) it to the wound surface can be problematic. A sugar paste is easier to apply. Gordon reported in 1985 sugar paste formulations (thin or thick paste variations) with antibacterial properties even when diluted by 50% from wound serum.
A commercial sugar paste (U-Pasta- Kowa Co. Ltd, Nagoya, Japan) containing 70% sugar and 3% povidone iodine was demonstrated to inhibit bacterial growth and promote re-epithelialization in one study. Applied liberally, a topical dressing and bandage are used to maintain the sugar paste in contact with the wound.
The numerous documented advantages of (Manuka) honey suggest it is a better choice than sugar. Nonetheless, sugar is an economical option that is readily available in the grocery store.
There are various honey dressings available for human use. The author currently uses Medihoney sterile dressings distributed by Dermasciences (licensed by Comvita Medical). This Manuka honey/alginate based dressing does not stick to the wound and is easily applied to flat wounds (See Figure 1).
Once a healthy granulation bed forms, surgical closure can be considered or open wound management continued with honey, sugar, or other topical products. Lastly, caution is required when using honey and sugar over large surface areas. Loss of fluid, protein, and electrolytes can be considerable, necessitating a close assessment of the patients.
Article modified from Pavletic MM. Atlas of Small Animal Wound Management and Reconstructive Surgery, 4th Edition. Wiley-Blackwell Publishers. Available for purchase April 2018.
Suggested References:
Baranoski, S, Ayello, EA. (2016). Wound Care Essentials: Practice Principles. 4th ed. New York: Wolters Kluwer.
Bryant RA, Nix DP. 2016. Acute and Chronic Wounds: Current Management Concepts, 5th ed. St. Louis: Elsevier Inc.
Mathews K, Binnington A. 2002. Wound management using sugar. Compend Contin Edu Pract Vet 24:41–50.
Mathews K, Binnington A. 2002. Wound management using honey. Compend Contin Edu Pract Vet 24:53–59.
Middleton KR, Seal D. 1985. Sugar as an aid to wound healing. Pharm J 235:757-758.
Thomas, S. (2010). Surgical Dressings and Wound Management. Cardiff, South Wales: Medetec Publications.