-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Referrals
- Referral Forms/Contact
- Direct Connect
- Referring Veterinarian Portal
- Clinical Articles
- Partners in Care Newsletter
CE, Internships & Alumni Info
CE Seminar Schedule
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 By Allison Allukian, DVM
By Allison Allukian, DVM
angell.org/emergency
emergency@angell.org
617-522-7282
Introduction
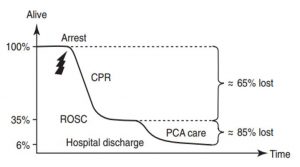
Cats and dogs have only a 6-7% rate of survival to discharge following cardio-pulmonary arrest (CPA).1,2 In CPA, there are two main phases of patient loss. The first phase is during initial CPA where the patient does not have return of spontaneous circulation (ROSC) in which about 65% of patients will be lost. The second phase of patient loss is after ROSC. Of those patients that have ROSC, about 85% will be euthanized or die before hospital discharge (Figure 1).1,2 It is during this time that interventional strategies after ROSC has the potential to save more lives. Given the complexity of these cases, post cardiac arrest patients require intensive monitoring in a 24 hour critical care facility to prevent re-arrest and to manage post cardiac arrest syndrome.
Post Cardiac Arrest Syndrome: Definition and Pathogenesis
Post cardiac arrest (PCA) syndrome is a complex pathological response that occurs as a sequela to global body ischemia followed by reperfusion. The four main components of PCA syndrome include brain injury, myocardial dysfunction, systemic ischemia/reperfusion injury, and pre-existing co-morbidities.2,3,4
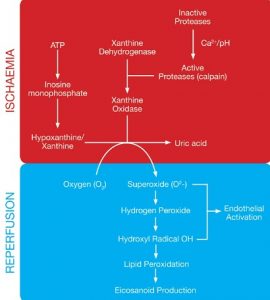
While ischemia creates the initial insult, paradoxically, it is the return of perfusion that causes further damage to the organ itself and may induce systemic damage to distant organs (Figure 2). Ischemia is when oxygen supply is less than the demand needed for normal tissue function.4 It results in anaerobic glycolysis and significantly decreased production of energy to two ATP + lactate. Elevating lactate levels will lower the pH in the tissue which feedbacks negatively to inhibit ATP production. ATP is broken down to hypoxanthine and xanthine, which later becomes important in reperfusion injury and the production of free radicals. With no ATP production, the Na-K ATPase and calcium membrane pumps no longer work. This results in an influx of intracellular water and cellular swelling.4 Increased intracellular calcium results in conversion of the enzyme xanthine dehydrogenase to xanthine oxidase. With the return of blood flow, there is an influx of oxygen into the tissues, which catalyzes xanthine oxidase to degrade hypoxanthine and xanthine, thus liberating the highly reactive superoxide anion (O2-) and uric acid as by-products. Superoxide is subsequently converted to the hydroxyl radical (OH-) and consequently results in peroxidation of the cell’s lipid membranes and results in the production and systemic release of pro-inflammatory eicosanoids, disruption of cell permeability and ultimately cell death.
Neuronal tissue is sensitive during anaerobic glycolysis, and will deplete its ATP resources within 2-4 minutes compared to 20-40 minutes in the gastro-intestinal tract and myocardium.2 Myocyte dysfunction results from ischemia and re-perfusion similar to what occurs at the cellular level in the nervous system.2 Neuronal injury can manifest as delirium to coma, seizures, myoclonus, cognitive dysfunction, cortical blindness or brain death. Myocardial dysfunction is characterized by increased central venous pressure and can clinically manifest as reduced cardiac output, arrhythmias, hypotension, cardiogenic shock or even cardiovascular collapse in severe cases.2, 3
Targeted Therapy
Monitoring of the post cardiac arrest patient uses the same principles as those you would apply to the critical patient. The goal immediately after ROSC is to sustain spontaneous circulation and perfusion of vital organs (i.e. brain, myocardium), attenuating further injury, and preventing re-arrest.
“Sepsis-like Syndrome”
Systemic ischemic-reperfusion injury is a sepsis-like syndrome because it shares many of its characteristics in relation to coagulation, inflammation and the endothelium. Treatment is highly individualized, but is similar to sepsis therapy and targeted at early hemodynamic optimization, glycemic control, and situational adrenal dysfunction (critical illness related corticosteroid insufficiency or CIRCI). Hemodynamic goals to reach are a mean arterial pressure of 80mmHg or higher, a central venous oxygen saturation of 70% or more, and a lactate less than 2.5mmol/L.5 Strategies include the administration of intravenous fluids with the addition of vasopressors, inotropes, and blood products to reach these goals with frequent re-assessment of these endpoints.2,3,5 Hyperglycemia is a common occurrence in human PCA patients and animal studies demonstrate that it worsens ischemic brain injury.3 Human studies have shown no difference in mortality between PCA patients with tight glycemic control (72-108 mg/dL) versus moderate (108-140mg/dL) glycemic control.3 Currently, moderate glycemic control is suggested for human PCA patients and a similar strategy in dogs and cats may be considered.2,3 While steroid administration in sepsis and PCA in humans is controversial, CIRCI has been identified in several human clinical studies after ROSC which has been associated with increased mortality.3,5 Administration of low-dose hydrocortisone in dogs and cats with vasopressor-dependent shock after CPA, with or without documented CIRCI, is reasonable.3,5
Neuroprotective Strategies
Mild therapeutic hypothermia (MTH) is recommended in patients that remain comatose after ROSC, if mechanical ventilation and advanced critical care capability is available. MTH helps attenuate further injury to both the brain and heart in PCA. In human medicine, patients are actively cooled between 89.8 to 920 F core body temperature with cooling blankets, ice packs, IV infusion of ice cold saline, and endovascular cooling devices. It is started immediately after ROSC but the ideal duration of MTH is unknown, with more severely injured patients likely to require longer duration. MTH is one of the only treatments proven in clinical trials to benefit patients with PCA due to its neuroprotective effects. It decreases mitochondrial injury, reduces cerebral metabolism, and decreases production of reactive oxygen species. In dogs and cats, the target MTH is the same as it is for people with slow rewarming (0.25 to 0.5oC per hour) if mechanical ventilation and critical capabilities are possible.5 These patients must be sedated, intubated and ventilated to avoid shivering and increased muscle tone. However, permissive hypothermia is an alternative in spontaneously hypothermic patients after CPA. The presence of coma absence pupillary light reflex 24-72 hours after ROSC significantly increases likelihood of poor neurological outcome.
Other neuroprotective strategies include monitoring for non-convulsive seizures (only identified by electroencephalography) and anti-convulsant treatment, as seizures increase cerebral metabolism and oxygen demand.
Myocardial Dysfunction
Myocardial injury and resulting dysfunction is also likely attenuated by hypothermia. Other than MTH, no other treatments have been identified to be clinically effective in attenuating myocardial dysfunction.4 Echocardiogram is used for diagnosis and serial echocardiograms for progression, response to treatment and resolution. Dobutamine administration is the treatment of choice for improving systolic function and output in both cats and dogs.2 Cardiac arrhythmias should also be addressed as needed based on their severity. Fortunately, myocardial dysfunction is reversible and typically resolves in 48 hours.
Re-oxygenation
While re-oxygenation after global ischemia is the goal of PCA care, controlled re-oxygenation is important to avoid both hypoxemia and hyperoxemia. Oxygenation guidelines recommend maintaining a fraction of inspired oxygen (FiO2) that produces an arterial oxygen saturation of 94-96%.5 In the early stages of reperfusion, hyperoxemia harms post-ischemic neurons by causing excessive oxidative stress. Evidence suggests that “arterial hyperoxemia soon after ROSC increases oxidative brain injury and neurodegeneration, and worsens functional neurological outcome and negatively impacts overall survival.”2
Positive pressure ventilation is not routinely recommended in all PCA patients, but is usually needed in the PCA patient that is hypoventilating or is unable to maintain normocapnia or normoxemia.5
Precipitating Factors
Persistent precipitating pathology and pre-existing co-morbidities will influence prognosis as they will persist after ROSC and add great variability to the PCA patient population. Limited information is available about what these factors are in small animal populations. Precipitating factors need an individualized approach using critical care principles to support oxygenation, ventilation, and circulation to realize a patient’s potential for a positive and meaningful outcome.
References
- Hoffmeister EH, et al. Prognostic indicators for dogs and cats with cardiopulmonary arrest treated by cardiopulmonary cerebral resuscitation at a university teaching hospital, JAVMA 235(1): 50-57, 2009.
- Boller M, et al. 2015. Post-Cardiac Arrest Care in Silverstein D. Small Animal Critical Care.
- Neumar, Robert W et al. Post-Cardiac Arrest Syndrome: epidemiology, pathophysiology, treatment, and prognostication. A consensus statement from the International Liaison Committee on Resuscitation (American Heart Association, Australian and New Zealand Council on Resuscitation.) Circulation 2008; 118 (23): 2452-2483.
- Cowled Prue et al. 2011. Pathophysiology of Reperfusion Injury in Fitridge R, et al, Mechanisms of Vascular Disease: A Reference Book for Vascular Specialists [Internet]. Adelaide (AU): University of Adelaide Press.
- RECOVER evidence and knowledge gap analysis on veterinary CPR. Part 7: Clinical Guidelines. Fletcher, Daniel J et al. Journal of Veterinary Emergency and Critical Care 22 (S1) 2012, p S102-S131.