-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 By Klaus Loft, DVM
By Klaus Loft, DVM![]()
angell.org/dermatology
dermatology@angell.org
617-524-5733
x
x
x
Introduction
Scabies is a very pruritic and crust-forming skin infection caused by closely related mites that affect many different species of animals and humans. The microscopic ectoparasitic mite causes scabies Sarcoptes scabiei (from Latin scabere, to scratch). This parasitic skin infection was the very first infectious disease agent affecting humans and animals ever identified and named in the literature.1–3 The parasite was fully identified and described in 1687 by the Italians Cestoni and Bonomo4 as Acarus. The name Acarus is accredited to Aristotle.5 Later, more accurate classification work renamed it as Sarcoptes scabiei (var. spp.) The skin disease is mentioned in the Bible by Leviticus, and similar parasites affecting sheep were described by Cornelius Celsus (25 BC-50AD),6 who recommended treatment with a mixture of sulfur and tar for the condition, similar to what was recommended in humans at the time. The human infection Sarcoptes scabiei var. hominis is now on the WHO list of neglected tropical diseases1 affecting more than 100 million people annually.
Canine Scabies
The obligate ectoparasite Sarcoptes scabiei var. canis is closely related to non-parasitic mites (See photos 1, 2, and 3) like the dust and storage mites (Dermatophagoides spp.)7,8 and to other veterinary relevant parasitic mites; Cnemidocoptes spp. (avian), Chorioptes spp. (ovine, equine, and bovine), Psoroptes spp.(bovine, caprine, equine, and ovine), Notoedres spp. (feline), and Otodectes spp. (cats, dogs, and others).
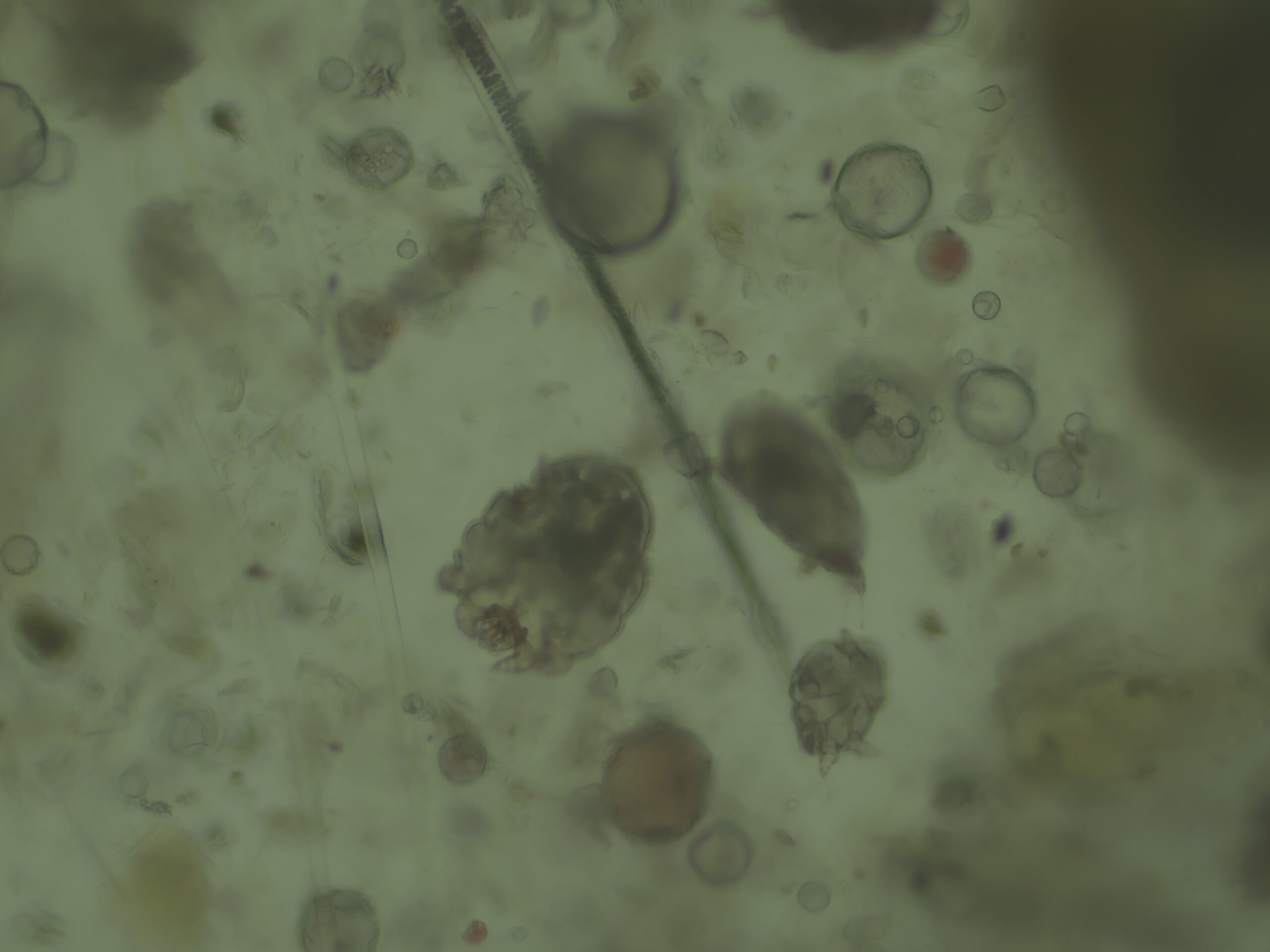
Photo 1
x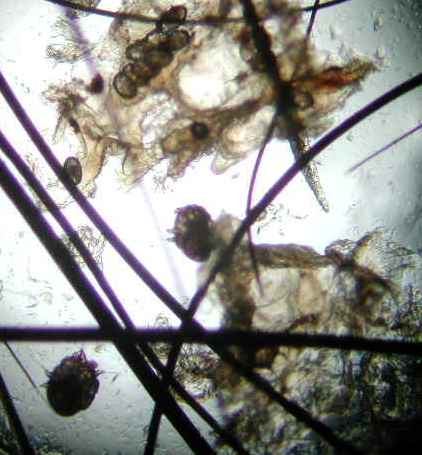
Photo 2
x
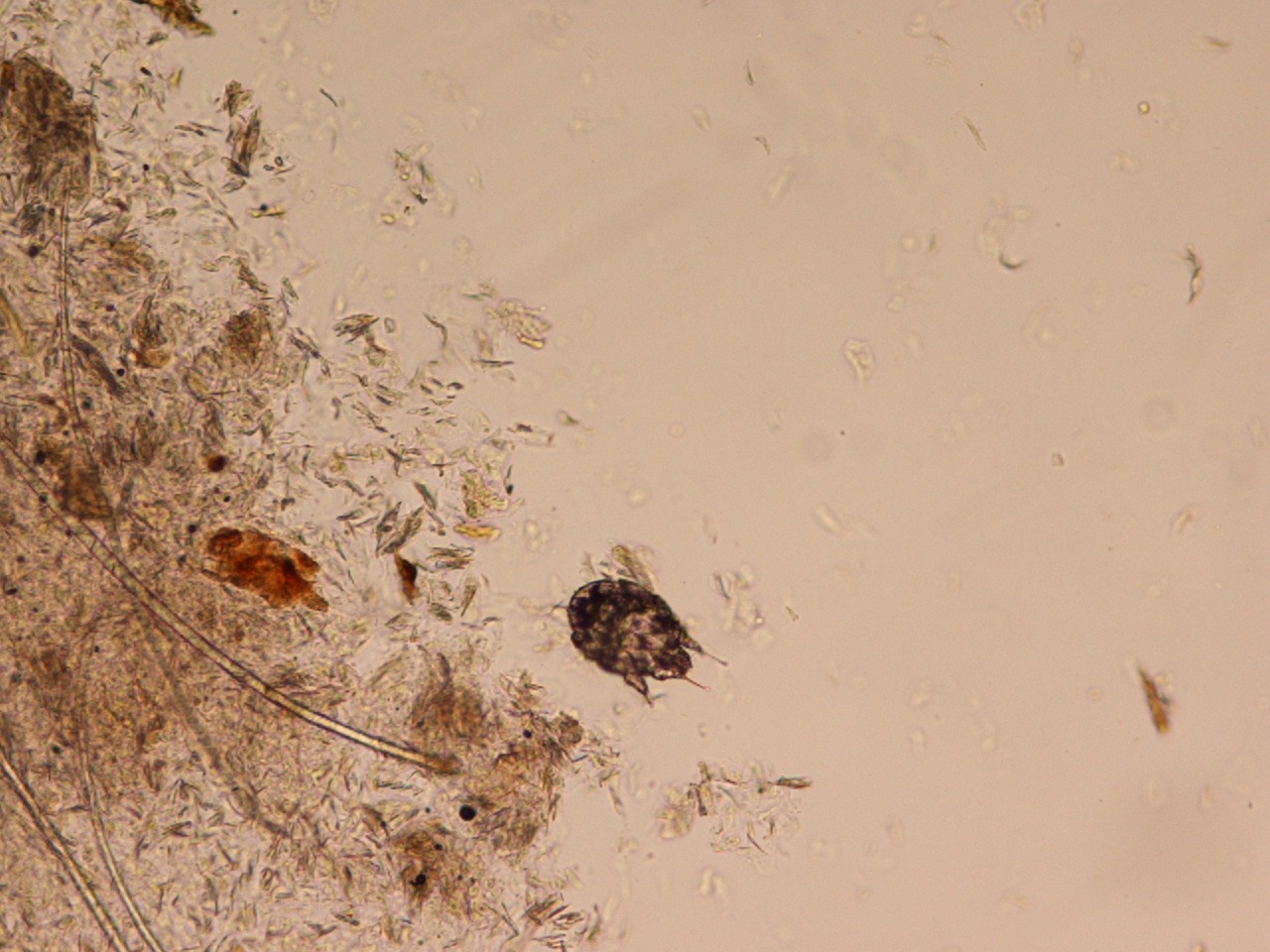
Photo 3
x
In today’s urban pet dog lifestyle, the parasite is most often spread via direct contact with infested dog(s) or from indirect contact with contaminated fomites (bedding, debris) with recent (likely less than 24 hrs) contact from infested related species (foxes, coyotes, wolves, and less likely bears and raccoons). In the past, dogs used for hunting would become exposed when being sent into foxholes or during transport. Foxes appear very susceptible to these parasites and can harbor mites in the thousands or more when severely infested, and might be a reservoir in many metropolitan areas. The old Greek word for fox is Alopou or Alopex (root of alopecia), likely due to the severe fur loss in this animal due to sarcoptic mange.
Diagnosis
The history is often highly suggestive of the infestation with pruritus of all dogs in close contact with the dog having similar intense pruritic symptoms). Clinical symptom distribution mainly affects the ventral aspect of the body (elbows, axillae, or hocks), face, and along the edges of the pinna (See photos 4, 5, and 6) rather than actual otitis externa involving the ear canals. The so-called positive pinnal-pedal reflex is present in 90% or more of infected dogs,9 and can be seen when firmly rubbing the edges of the pinna and the hind leg involuntarily starts to pedal. Although this highly supports a diagnosis, it does not confirm the infection since the same reaction can occur with atopic and flea-allergic dogs.10 Confirming a true infection can be done by performing several superficial skin scrapes with mineral oil and examining the debris under a microscope.

Photo 4
x

Photo 5
x

Photo 6
x
Additionally, serology testing for mite IgE is highly sensitive and specific but less commonly used in the US.9,11,12 The mites often exist in low numbers in the epidermis of dogs and can be challenging to find. Extensive skin scraping often shows no mites or eggs (See previous photos 1, 2, and 3) and can create a “false negative” result. If sarcoptic mange is suspected, empirical treatment may be the only way to diagnose and cure the dog. Immune-compromised patients might be at increased risk of developing more severe levels of parasitic infection.
This disease is highly contagious and can spread from pet to pet or from pet to human. While canine sarcoptes mites can bite humans, they rarely cause full-blown disease in humans. All dogs in the household should be treated whether or not they have symptoms. If any family members have red itchy bumps on their skin, they should consult their physician.
Treatment13
Several medicines can kill the sarcoptes mites after they have hatched. These include topical and oral forms. The options listed below all have a role in referral practice; for most general practice using the newer generations of oral flea and tick prevention is the best place to start.
- Isoxazoline (afoxolaner, sarolaner, lotilaner &) (Nexgard®1, Credelio®*, Simparica®*TRIO, Bravecto®*): These are part of a new class of chewable anti-parasitic drugs used primarily for flea and tick prevention for dogs and cats. Very effective and very limited risk of side effects, some anecdotes about known seizure patients being at increased risk of seizure activity after starting these types of products. Some indirect evidence has suggested these could be used even in heartworm-positive animals. We recommend having a negative heartworm test before use.
- Selamectin (Revolution® Plus): This is an FDA-approved treatment for sarcoptic mange in dogs and is safe for cats. Additionally, it appears safe in dogs with MDR-1/ABCB1 mutation as it is not a p-glycoprotein substrate.14 Rapid parasitic adulticide effect, recommend using in patients with recent negative heartworm test or continuous, high-quality heartworm prevention having been used.
- Moxidectin (Advantage® Multi) Bravecto®*, Simparica®*TRIO, ProHeart®, etc.: FDA-approved treatment for sarcoptic mange in dogs and heartworm preventative that has been very effective in the treatment of sarcoptes. It is available as a liquid spot-on and as an oral tablet form in combo with fluralaner (see below) for dogs and topical for cats; both are effective against fleas, otodectes, demodicosis, heartworms, and some intestinal parasites. Rapid parasitic adulticide effect recommends use in patients with a recent negative heartworm test or continuous, high-quality heartworm prevention having been used.
- Ivermectin (Ivomec®): This is a livestock endo- and ecto-antiparasitic, available as a liquid deworming agent, effective for sarcoptic mange; the same drug is used in lower dosages for heartworm prevention in Heartgard®. Dogs with MDR-1/ABCB1 mutation, especially herding breed dogs, have a CNS sensitivity due to a blood-brain p-glycoprotein causing the inability to remove ivermectin from the CNS space. Signs of toxicity include sedation, drooling, loss of balance, vomiting, seizures, rarely blindness, and coma. High-risk breeds can be PCR tested for this mutation.15 This has become a less frequently used option but can be helpful in large outbreaks of low MDR risk breeds (kennels, shelters, etc.)
- Milbemycin oxime (Interceptor®): Milbemycin is available as a heartworm preventive in combination with flea prevention lufenuron for dogs. When given at a higher dose, milbemycin is also effective for treating sarcoptic mange. Some dogs, especially herding breed dogs, can be sensitive to high doses of milbemycin. Signs of milbemycin sensitivity are similar to those of ivermectin but occur less frequently. Milbemycin is a very safe option in most scenarios but expensive.
- Lime sulfur dip (LymDip) and Amitraz dips (Mitaban): These are older but still effective ectoparasitic treatments but are seldom used today due to odor and staining of the fur coat, paint, wood, jewelry, or porcelain. They should be considered for patients where the systemic options mentioned above would be contraindicated.
No matter which treatment is chosen, no current treatments will kill the egg stages of the parasite. The positive patient may remain contagious for two to four weeks after the initial treatment. Sarcoptes mites can only survive a short time off of a host, but a female scabies mite in an untreated animal can live for up to two months in the epidermis and lay up to one to two eggs per day. The patient suffers from severe pruritus, often complicated with secondary bacterial and/or yeast superficial to deep pyoderma.5 Many commonly used anti-pruritic treatments like anti-histamines, steroids, JAK-stat inhibitors, or IL-31 monoclonal anti-body treatments will likely only be partially effective in controlling parasitic pruritus. Recently infected individuals might have false positives or extra high results for dust and storage mites if allergy tested within two to three months of sarcoptes resolution due to the similar immune response in the host with exposure to those mites.
References
- El-Moamly AA. Scabies as a part of the World Health Organization roadmap for neglected tropical diseases 2021-2030: what we know and what we need to do for global control. Trop Med Health. 2021;49(1):64. Accessed September 21, 2021. http://www.ncbi.nlm.nih.gov/pubmed/34399850
- Holt DC, Fischer K. Novel insights into an old disease: Recent developments in scabies mite biology. Curr Opin Infect Dis. 2013;26(2):110-115. doi:10.1097/QCO.0B013E32835EB986
- Thomas C, Coates SJ, Engelman D, Chosidow O, Chang AY. Ectoparasites: Scabies. J Am Acad Dermatol. 2020;82(3):533-548. doi:10.1016/j.jaad.2019.05.109
- Roncalli RA. The history of scabies in veterinary and human medicine from biblical to modern times. Vet Parasitol. 1987;25(2):193-198. doi:10.1016/0304-4017(87)90104-X
- Currier RW, Walton SF, Currie BJ. Scabies in animals and humans: history, evolutionary perspectives, and modern clinical management. Ann N Y Acad Sci. 2011;1230(1). doi:10.1111/j.1749-6632.2011.06364.x
- The Editors of Encyclopaedia Britannica. Aulus Cornelius Celsus | Roman medical writer | Britannica. www.britannica.com. Accessed November 13, 2022. https://www.britannica.com/biography/Aulus-Cornelius-Celsus
- Arlian LG. Biology, Host Relations, and Epidemiology of Sarcoptes scabiei. Annu Rev Entomol. 1989;34(1):139-159. doi:10.1146/annurev.en.34.010189.001035
- Arlian LG, Morgan MS. A review of Sarcoptes scabiei: Past, present and future. Parasites and Vectors. 2017;10(1). doi:10.1186/s13071-017-2234-1
- Mueller RS, Bettenay S V., Shipstone M. Value of the pinnal-pedal reflex in the diagnosis of canine scabies. Vet Rec. 2001;148(20):621-623. doi:10.1136/vr.148.20.621
- Hensel P, Santoro D, Favrot C, Hill P, Griffin C. Canine atopic dermatitis: Detailed guidelines for diagnosis and allergen identification. BMC Vet Res. 2015;11(1). doi:10.1186/S12917-015-0515-5
- Lower KS, Medleau LM, Hnilica K, Bigler B. Evaluation of an enzyme-linked immunosorbant assay (ELISA) for the serological diagnosis of sarcoptic mange in dogs. Vet Dermatol. 2001;12(6):315-320. doi:10.1046/j.0959-4493.2001.00265.x
- BORNSTEIN S, ZAKRISSON G. Humoral Antibody Response to Experimental Sarcoptes scabiei var. vulpes Infection in the Dog. Vet Dermatol. 1993;4(3):107-110. doi:10.1111/j.1365-3164.1993.tb00202.x
- Plumb D. Plumb’s Veterinary Drugs. Published online 2018:1456. Accessed January 31, 2021. https://www.plumbsveterinarydrugs.com/home2/
- Mealey KL. Canine ABCB1 and macrocyclic lactones: Heartworm prevention and pharmacogenetics. Vet Parasitol. 2008;158(3):215-222. doi:10.1016/j.vetpar.2008.09.009
- Geyer J, Döring B, Godoy JR, Moritz A, Petzinger E. Development of a PCR-based diagnostic test detecting a nt230(del4) MDR1 mutation in dogs: Verification in a moxidectin-sensitive Australian Shepherd. J Vet Pharmacol Ther. 2005;28(1):95-99. doi:10.1111/j.1365-2885.2004.00625.\
[1] Extra-label use for sarcoptes, not FDA approved.