-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Referrals
- Referral Forms/Contact
- Direct Connect
- Referring Veterinarian Portal
- Clinical Articles
- Partners in Care Newsletter
CE, Internships & Alumni Info
CE Seminar Schedule
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 By Michael M. Pavletic, DVM, DACVS-SA
By Michael M. Pavletic, DVM, DACVS-SA
![]() angell.org/surgery
angell.org/surgery
surgery@angell.org
617-541-5048
October 2023
x
x
Common Causes of Wound Dehiscence
Wound dehiscence, or the disruption of apposed surfaces of a wound, is the result of several factors, either alone or in combination. Dehiscence is one of the most common postoperative complications encountered by veterinarians. The resultant costs associated with wound care and closure can easily double the cost of the original surgery. Fortunately, most of the causes of wound dehiscence are preventable.
The following are the most common causes noted by the author:
- Wound closure under excessive tension, with suture “cut-out,” secondary to ischemic necrosis
- Suture placement too close to the incisional border with “cut-out” (collagenase activity
within 5 mm cutaneous zone bordering skin incision) - Improper suture material selection (size, tensile strength, suture pattern, placement,
rate of resorption/degradation)
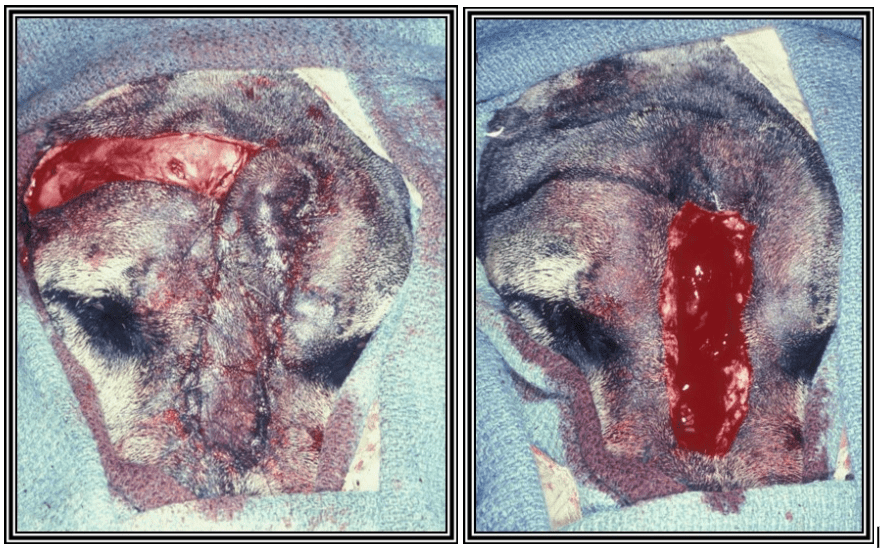
Bite wound on dog with closure of compromised tissue
- Closure of severely compromised skin with subsequent necrosis
- Suture placement, compromising cutaneous circulation
- Moisture accumulation contributes to tissue overhydration and maceration
- An underlying pocket of infection, necrosis, foreign body, or neoplasia
- Lack of postoperative protection/support from motion, licking, and external trauma
- Premature suture removal
- Delayed healing precipitated by corticosteroids and other agents
- Suture placement in scar tissue, which has poor suture-holding ability
- Excluding the above causes, an underlying healing disorder or delay in healing should be suspected
Key Clinical Points
Critical evaluation of the separated wound can assist the surgeon in determining the most likely cause(s) of dehiscence. Incisional gaps with the absence of sutures suggest the premature removal of sutures, usually by the patient. The presence of the sutures oftentimes demonstrates a suture “cut-out” from one side of the incision, with an irregular right-angle tear from the suture hole to the incision. An intact suture with the presence of an incisional gap is usually associated with stretching or deformation of suture material (from incisional tension or sutures deliberately placed loosely. Often, a veterinarian may place sutures loosely when edema of the skin is evident or anticipated. When the swelling subsides, the incisions retract, leaving an incisional gap.

Directing skin to reduce incisional tension
Suture “cut-out” can occur from placement too close to the incision. Because collagenase activity remains high within 5 mm of the skin incision, sutures placed near or within this zone are more likely to cut-through the weakened dermal collagen weave, especially in the presence of motion and incisional tension. Larger suture bites are less likely to pull out. Cutting needles have a cutting edge within the curvature of the needle. Under tension, with placement in susceptible skin, the suture is more likely to cut along the “V” shape cut created by the suture in the direction of the incision. Today, most surgeons use reverse cutting needles (cutting edge on the outer curvature of the needle) almost exclusively since the flat edge of the needle hole facing the incision line is more resistant to tissue tear.
For example, delays in healing from inflammation, trauma, or malnutrition will further increase the likelihood of dehiscence. Suture placement, pattern, and selection are particularly important under these circumstances. At the time of traumatic wound closure, it is not always clear whether the onset of necrosis resulted from “dying skin” or additional ischemia precipitated by tight suture placement. Large areas of skin necrosis would suggest preceding trauma was primarily responsible for dehiscence. In areas with ample regional skin, aggressive debridement could prevent dehiscence by removal of compromised or potentially compromised tissues. Necrosis limited to the suture site would be compatible with suture compromise to the skin.
Selecting an elastic suture material that can stretch to a limited degree to accommodate possible tissue swelling but is of sufficient size and strength to prevent permanent stretch deformation is useful. Suture material size and selection should be tailored to the skin thickness, durability, location, and the anticipated postoperative incisional forces that require neutralization. In more difficult wound closures, complete familiarity with the physical properties of a given suture material is essential for more consistent success in wound closure.
Closure of an incision under moderate tension increases the likelihood of dehiscence. Closure under tension, with the addition of motion, can further promote suture serration of the skin and “cut-out.” Techniques to offset skin tension should be considered in concert with immobilization of the area to promote uncomplicated healing. [Closure of wounds under excessive tension is the most common cause of wound dehiscence.]
Transposition flap closure (before and after)
Underlying pockets of infection, necrotic tissue, or foreign bodies will result in persistent wound drainage at the expense of incisional closure until the underlying causes are alleviated. Future continuous discharge and prolonged moisture exposure can hydrate or soften the skin, enhancing the likelihood of suture cut-out. As a result, failure to abide by basic wound management principles can negatively affect wound healing and closure until the problems are recognized and remedied.
Proper bandage and external support can be critically important to preventing dehiscence in areas subject to motion or weight-bearing. Care and proper bandage care are used to avoid circulatory compromise during bandage application.
Surgical Options to Reduce Surgical Tension
- Careful undermining
- Release or relaxing incisions
- Load cycling with skin hooks — intraoperative skin stretching
- Tacking sutures, including walking sutures
- Skin flaps
- Skin stretchers (Contact Dr. Pavletic if needed)
Open Wound Management
The area of dehiscence is thoroughly examined to determine what factors likely led to this complication. Those identifiable causes will need to be eliminated.
With wound dehiscence, the condition of the tissues is evaluated for tissue necrosis and the presence of infection. Debridement and a variable period of open wound management may be required before surgical closure can be attempted. Depending on the size and location of the wound, healing by second intention may be the best option.
As noted, closure under tension is the most common cause of wound dehiscence. Surgical methods to reduce tension of the closure should be considered, along with the appropriate immobilization of the area if motion is a contributing factor.
x
Reference
- Pavletic MM. Atlas of Small Animal Wound Management and Reconstructive Surgery, 4th ed. Wiley Blackwell, 2018.