-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Referrals
- Referral Forms/Contact
- Direct Connect
- Referring Veterinarian Portal
- Clinical Articles
- Partners in Care Newsletter
CE, Internships & Alumni Info
CE Seminar Schedule
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 Unfortunately, accidents and medical emergencies can happen to our pets, and as responsible owners, it is our duty to be as prepared as possible and act as first responders. Dr. Jordana Fetto, DVM, who specializes in Emergency and Critical Care at the MSPCA-Angell West in Waltham, advises on some common pet first aid emergencies, offers tips on prevention, and recommends how to create your own pet first aid kit.
Unfortunately, accidents and medical emergencies can happen to our pets, and as responsible owners, it is our duty to be as prepared as possible and act as first responders. Dr. Jordana Fetto, DVM, who specializes in Emergency and Critical Care at the MSPCA-Angell West in Waltham, advises on some common pet first aid emergencies, offers tips on prevention, and recommends how to create your own pet first aid kit.
Advice for Common First-Aid Emergencies
Your pet is poisoned
If you think your pet has ingested something poisonous, the first step is to call ASPCA Poison Control at 888-426-4435 or the Pet Poison Helpline at 855-764-7661. Please be aware that a consult fee may apply!
You will be asked to provide information about your pet:
- Species
- Breed
- Age
- Weight
- Existing medical conditions (if any)
- Medications your pet currently takes
“You will also be asked to provide the name of the product your pet was exposed to and possibly the list of active ingredients, the amount your pet was exposed to, how much time has passed since exposure, and if your pet is currently showing any symptoms of illness (e.g., vomiting, tremors, seizures, loss of consciousness),” said Dr. Fetto.
Depending on your pet’s species and weight, as well as the type and amount of toxin consumed, ASPCA Poison Control will inform you if the substance is indeed toxic, if a toxic dose was ingested, and the next steps of either inducing vomiting at home or bringing your pet to the closest veterinary emergency room.
“Since you may be directed to induce vomiting at home, it is important to have fresh 3% hydrogen peroxide in your medicine cabinet,” said Dr. Fetto. “Do not give hydrogen peroxide unless directed to by a veterinarian or Poison Control. Ensure the product is available to provide the correct name, list of active ingredients, and concentration for poison control.”
If your pet’s skin or eyes were exposed to a caustic substance, check the label for instructions on how to treat a human if exposed. If the recommendation is to wash the skin, Dr. Fetto recommends using Dawn dish soap to wash your pet, making sure to avoid contact with the eyes, nose, and mouth. If instructed, flush the skin or eyes immediately with water or saline eye rinse.
Common household poisons
Foods
- Xylitol (i.e., wood sugar, birch sugar, birch bark extract) is a sugar-free ingredient found in products such as chewing gum and drinks.
- Raisins/grapes
- Onion/garlic (fresh, paste, powder)
- Chocolate
- Caffeine
- Alcohol
- Raw yeast dough
- Macadamia nuts
Plants
Many plants are toxic, and symptoms range from mild stomach upset to life-threatening kidney failure and arrhythmias. Thus, checking the ASPCA list of toxic and non-toxic plants before bringing plants inside your home or landscaping your yard is important.
list of toxic and non-toxic plants before bringing plants inside your home or landscaping your yard is important.
Examples of common toxic plants include:
- Lilies (kidney failure)
- Sago palms (liver failure and coagulopathy)
- Azaleas (heart failure)
Household Products
- Antifreeze
- Cleaning products
- Pesticides
- Compost and fertilizers
- Rodenticides
Medications
Over-the-counter medications, especially non-steroidal anti-inflammatory medications such as ibuprofen and naproxen, are the most common toxins pets are exposed to. These can result in severe gastrointestinal signs, kidney failure, and neurologic signs. As you do with children, keep all medications—over-the-counter and prescription—out of reach from your pet.
Your pet is injured or bleeding
Fractures
If you suspect your pet has sustained a fracture, you can try to stabilize the injury by placing a bandage or splint. “A poorly placed splint/bandage can do more harm than good, so if you are uncertain about your ability to place the splint, skip this step,” said Dr. Fetto.
Instead, transport your pet to a veterinarian for pain medication and radiographs to confirm the fracture and splint placement. While transporting your pet, keep them confined in a small area (e.g., a pet carrier, box, or another container) to reduce the risk of further injury. For large dogs, you can use a sled, blanket, or something similar to act as a stretch to facilitate transportation to and from your car.
Internal bleeding
Signs that your pet is suffering from internal bleeding include:
- Lethargy
- Collapse
- Pale pink to white gum color
- Bloody urine
- Bloody or black tar-like stool
- Bruising
- Bleeding from the nose, mouth, or rectum
- Coughing or vomiting up blood
“If you suspect your pet has internal bleeding, keep your pet as warm and quiet as possible and immediately bring him/her to the closest veterinary hospital,” said Dr. Fetto.
External wounds
If your pet has suffered an external wound and is bleeding, use a clean cloth or towel to apply firm pressure directly over the wound. Avoid removing the cloth to see if the bleeding has stopped until pressure has been applied for at least three minutes. “If bleeding is soaking through the cloth originally applied, DO NOT remove it,” explained Dr. Fetto. “Instead, layer additional towels on top of the original to prevent disturbing any blood clots that may have formed.” Seek veterinary care immediately, as your pet may require pain medications, antibiotics, and wound cleaning and closing.
Burns
If your pet has sustained a burn, flush the area with room temperature (NOT COLD) water to stop the thermal injury from spreading. Cover the burned area with a towel dampened with room-temperature water. Seek veterinary care immediately.
Eye injuries
Eye injuries can threaten your pet’s vision, are painful, and quickly worsen. “If you see a foreign object (e.g., a grain of sand or grass) in your pet’s eye, you can try using saline eye flush to rinse it out,” suggested Dr. Fetto. “But avoid trying to grab it with your fingers or tool, as further injury may result.” Apply an Elizabethan collar to your pet to prevent them from pawing at the eye or rubbing it on the ground or furniture, resulting in further  injury, and seek veterinary care immediately.
injury, and seek veterinary care immediately.
Animal bites
If an animal bites your pet, seek veterinary care immediately! If the attacking animal is someone’s pet, try to obtain the owner’s name, phone number, address, and the rabies vaccine status of the attacking animal.
If a snake bites your pet, assume it is venomous and seek veterinary attention immediately. Do not try to catch the snake! Instead, try to take a picture of the snake so the veterinarian can determine if it is one of the two venomous species in Massachusetts (the Northern Copperhead and the Timber Rattlesnake).
Your pet has heatstroke
Heat stroke can develop from a long walk on a hot day, leaving a pet in the car, or being out in the sun on a hot day without access to shade or water. Animals with pre-existing breathing problems (e.g., laryngeal paralysis) or brachycephalic breeds (e.g., English Bulldogs, French Bulldogs, Pugs) are at higher risk for developing heat stroke, but it can happen to any breed.
Signs of heat stroke:
- Heaving
- Breathing or panting
- Excessive drooling
- Nausea
- Vomiting
- Diarrhea
- Dry or sticky gums that may be an abnormal color
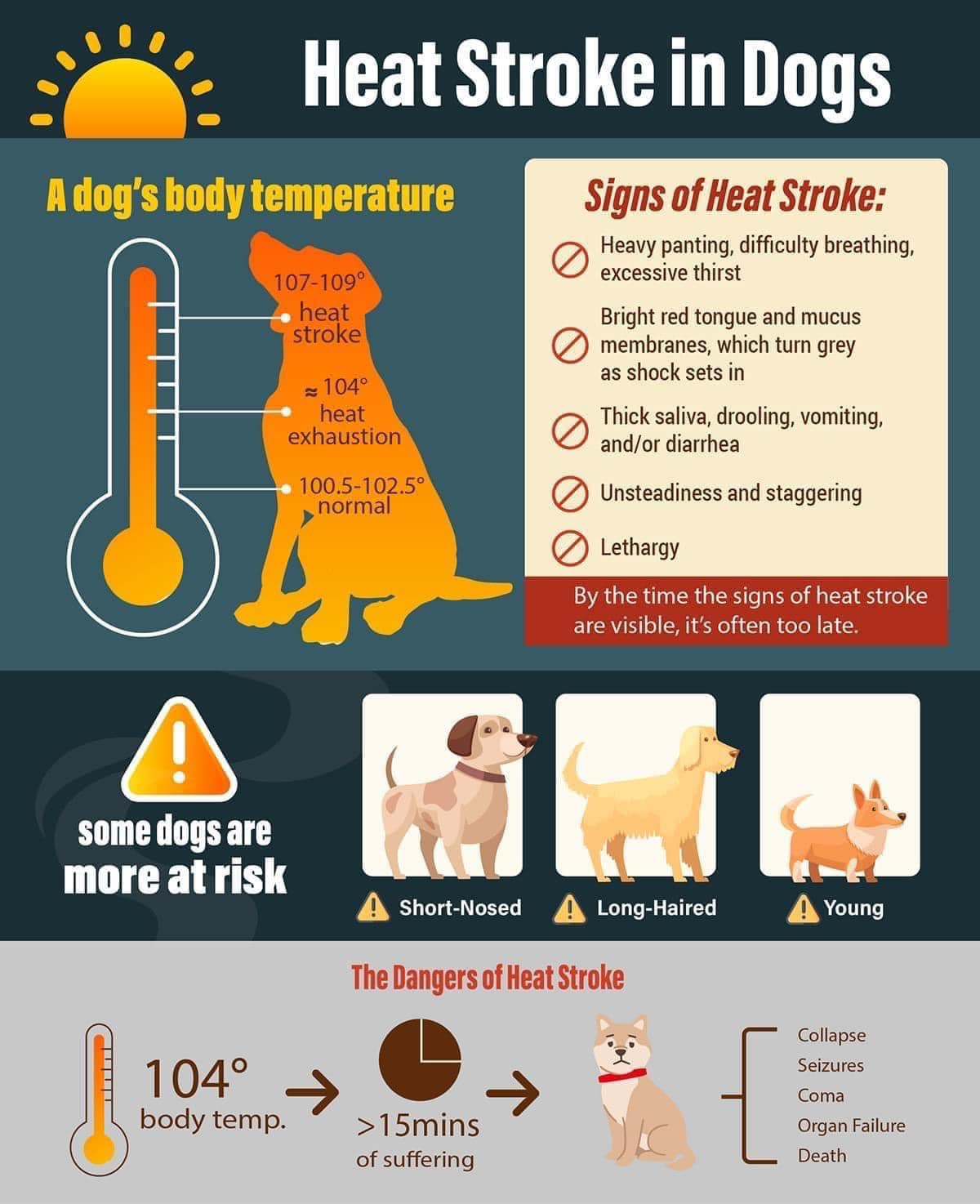
- Weakness, confusion, and collapse
If you suspect your pet is suffering from heat stroke, immediately bring them to the closest emergency veterinary hospital for evaluation and treatment. If your pet is in a hot environment, move them to a cool, shaded location. If your pet is alert, you can offer them water. If possible, place a fan on your pet and cover your pet’s neck, armpits, and groin with towels soaked in room-temperature water. Frequently resoak and replace the towels. “It is very important not to use cool or cold water, which can worsen their condition,” warned Dr. Fetto.
Your pet goes into shock
Shock is caused by extreme freight or injury. Classic signs of shock include nervousness, shallow breathing, a dazed, glassy eye appearance, pale gum color, and weak pulses. Keep your pet quiet and restrained in a safe area and warm with blankets. Seek veterinary care immediately.
Your pet is having a seizure
Most seizures are self-limiting and resolve within 30 seconds to two minutes. “If your pet has a seizure, keep them safe from sharp objects/furniture or stairs to prevent injury. Do not try to restrain your pet or place your hand in your pet’s mouth. If able, time the length of the seizure,” said Dr. Fetto.
Any seizure lasting more than three minutes, your pet has three or more seizures in 24 hours, or you must seek immediate veterinary attention if your pet doesn’t stop seizing. For up to 24 hours following a seizure, your pet may be disoriented, sleepy, unsteady on their feet, transiently blind, or ravenously hungry. If your pet has a known seizure disorder, once the seizure has resolved and your pet is alert and able to swallow safely, you may administer a dose of the anti-seizure medication. This is an extra dose given, and your pet’s normal medication dose and schedule should not be altered unless directed by a veterinarian.
Your pet is choking
 Signs that your pet is choking include difficulty breathing, pawing at their mouth or neck, making choking sounds when breathing or coughing, and blue-tinged lips or tongue.
Signs that your pet is choking include difficulty breathing, pawing at their mouth or neck, making choking sounds when breathing or coughing, and blue-tinged lips or tongue.
“If your pet can still breathe, try your best to keep them calm and seek veterinary care immediately,” said Dr. Fetto. If possible, open your pet’s mouth and look inside for a foreign object without risking injury to yourself. Gently try to remove the object if you can visibly see it. Be careful not to push it further down your pet’s throat.
For objects that cannot be removed from cats and small dogs, gently pick them up by the thighs and swing them upside down, side to side, to help dislodge the object. If this is unsuccessful, stand your pet on the ground and apply forward pressure to the pet’s abdomen behind the ribcage, similar to the Heimlich maneuver. For larger dogs where the object cannot be manually removed, perform the above-mentioned Heimlich maneuver. Seek veterinary care immediately!
Your pet is not breathing
“Stay calm and open your pet’s mouth,” said Dr. Fetto. “Pull the tongue forward so the tip is outside the mouth, and look inside the mouth for a foreign object blocking the airway. Remove the object gently to avoid lodging it further into the airway if you can see it.” If this elicits a response from your pet, stop. Use caution to avoid being bitten and then start providing rescue breaths:
- Lie your pet flat on the floor or table with the neck in neutral alignment
- Close your pet’s mouth with your hand and breathe directly into their nose until their chest expands. Your mouth will form a seal over both of your pet’s nostrils to ensure air goes to their lungs. You will need to blow forcefully and quickly.
- Allow the pet to exhale before administering the next breath.
- Give ten breaths per minute until your pet is breathing alone or you have arrived at a veterinary emergency hospital.
Even if your pet resumes breathing on its own, they will need to be evaluated by a veterinarian.
Your pet keeps vomiting and can’t keep down food or water
If your pet vomits a couple of times, you can try withholding food and water for 12 hours to allow the stomach upset to pass. If your pet has no additional episodes of vomiting during the fasting period, you can offer a bland diet of boiled chicken and rice. In mild cases of vomiting, you can also try administering Omeprazole (aka Prilosec), an over-the-counter antacid. Do not syringe food or water to your pet, as this could lead to aspiration pneumonia.
additional episodes of vomiting during the fasting period, you can offer a bland diet of boiled chicken and rice. In mild cases of vomiting, you can also try administering Omeprazole (aka Prilosec), an over-the-counter antacid. Do not syringe food or water to your pet, as this could lead to aspiration pneumonia.
“If your pet does not improve in the above scenario, has profuse vomiting with the inability to keep down food or water, or, especially a large breed dog, is non-productively retching, do not attempt management at home,” warned Dr. Fetto. “Instead, a veterinarian should evaluate your pet immediately—they may have a life-threatening condition.”
Your pet is stumbling and walking around “drunk”
A pet that is stumbling around and walking like they’re drunk may be suffering from an inner ear infection, vestibular disease, herniated intervertebral disc, low blood sugar, toxicity (i.e., xylitol, marijuana), or stroke, to name a few possible causes.
It is important to keep your pet from injuring themselves by not allowing them to walk up or down stairs unassisted or on slippery surfaces. “If you do not have a harness at home, you can use a rolled-up towel or small blanket as a sling under your pet’s chest and groin,” suggested Dr. Fetto. It is also important to seek veterinary care to determine and address the underlying cause.
Your pet has no heartbeat
If you believe your pet to be unresponsive, try to stimulate them by petting them or making a noise. If your pet does not respond and you notice they don’t have a heartbeat, begin CPR. The chances of your pet surviving cardiac arrest with resuscitation are very low, but this may be your pet’s only chance, so it is worth attempting.
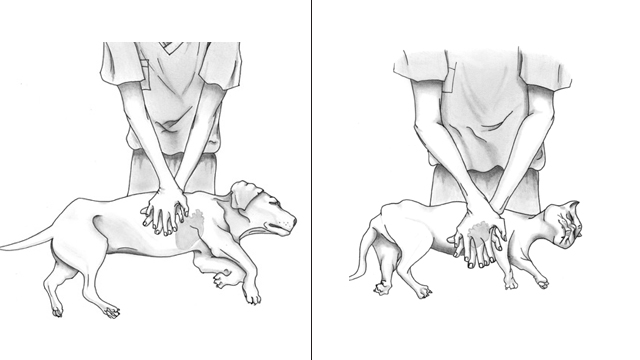
- For most cats and dogs, lay them on their side to perform chest compressions while you stand or kneel behind them.
- For small dogs and cats, use one hand to encircle the bottom of their chest between your thumb and fingers and squeeze.
- For other dogs, place your hands, one on top of the other with fingers interlaced, over the widest part of the chest and press down, keeping elbows locked, bending at the waist.
- Barrel-chested dogs (e.g., English Bulldogs) should be placed on their back with your hands on the breastbone, pressing down with elbows locked. In all three scenarios, the goal is to compress the chest ⅓ of its total width and allow for full recoil before administering the next compression at a rate of 100-120 compressions per minute.
- A helpful trick is administering compressions to the beat of the Bee Gees song “Stayin’ Alive.”
Focus your efforts on chest compressions. If you have another person with you, one person will perform chest compressions while the other provides rescue breathing.
Alternate tasks every two minutes to prevent fatigue and ensure quality chest compressions.
Continue chest compressions +/- rescue breathing until you can feel your pet’s heartbeat and breathe regularly on their own or until you have arrived at the closest veterinary hospital.
 DIY First Aid Kit for Pets
DIY First Aid Kit for Pets
You should have a first aid kit on hand for the humans in your household, and your pet needs one, too! Dr. Fetto does warn, however, “Before administering first aid, make sure you and your pet are in a safe place and use safety items (e.g., muzzles, e-collar, towels) to prevent your pet from biting you,” she says. “Keep your pet warm and minimize movement as much as possible if there is visible trauma.” And the most important point to remember is that first aid does not substitute veterinary care, and a veterinarian should evaluate your pet!
Important phone numbers and paperwork
- Your primary care veterinarian
- ASPCA Poison Control or Pet Poison Helpline
- Local animal control
- Local veterinary urgent cares
- Local emergency veterinary hospitals
- Please provide a copy of your pet’s medical record (including a list of current medications and the times they are administered) and the most recent rabies vaccine certificate.
Prescriptions
If your pet takes prescription medications, ensure that at all times, at least a week’s worth of medication is available. Please give the veterinarian and pharmacy at least three days to approve and fill your refill request.
If your pet is fed a prescription diet, make sure to have an extra bag of dry food or case of wet food on hand at all times, as it is possible to encounter delays when refilling it.
Over-the-Counter Medications
- Benadryl (Diphenhydramine) -An antihistamine. For treatment of mild allergic reactions.
- Prilosec (Omeprazole) – An antacid. For treatment of a mild upset stomach.
First Aid Supplies
- Water dish
- Spare leash and collar
- Warming blanket
- Towel
- Digital thermometer
- Flashlight
- Scissors with blunt ends
- Large syringe without needle or eye dropper to administer oral medications or clean wounds
- Tweezers
- Muzzle to prevent bite (DO NOT muzzle if your pet has been vomiting)
- Elizabethan collar or similar device
- Instant ice pack
- Kwik Stop powder
- Wound cleaning
- Box of latex gloves
- 4 x 4 gauze
- Q-Tips
- Chlorhexidine solution or saline solution- for cleaning wounds
- Artificial tears (e.g., Bausch & Lomb Eye Wash Relief Solution)- for cleaning out the eyes
- Triple Antibiotic Ointment (small amounts of Neosporin are ok for dogs but DO NOT USE for cats – Neosporin is toxic to cats)
- Bandage material – Choose the appropriate size for your pet, as these materials come in different widths.
- Cast padding
- Cling wrap
- Vet wrap
x
x
“It’s important to understand basic first aid techniques and assess what is beyond your comfort level and when to seek veterinary care emergently,” said Dr. Fetto. In addition to the information above, she suggests pet owners take the Red Cross First Aid course, “Cat and Dog First Aid Online Training.” And most importantly, do not hesitate to bring your pet to the nearest emergency veterinarian when the injury is beyond your control and needs immediate help. (Tip: call ahead to give staff a heads-up that you’re coming!)
24/7 Emergency & Critical Care at the MSPCA-Angell in Boston
Angell Animal Medical Center
350 S. Huntington Ave.
Boston MA 02130
617-522-7282
24/7 Emergency & Critical Care at the MSPCA-Angell West in Waltham
Angell West
293 Second Avenue
Waltham, MA 02451
781-902-8400



