-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 By Martin Coster, DVM, MS, DACVO
By Martin Coster, DVM, MS, DACVO
www.angell.org/eyes
ophthalmology@angell.org
617-541-5095
The word “cataract” derives from the Greek word for waterfall, and so is apt as the term for an opaque, whitened lens which impairs the passage of light (a more complete discussion can be read here). The lens is essentially a bag of protein, with lens fibers residing inside a defined capsule (a modified basement membrane). Like cooking an egg white, changes in the structure and orientation of the usually-parallel lens fibers will cause light to reflect from the surface, instead of transmitting through to the retina. Cataracts are typically staged from incipient (<10%) to immature (10-90+%) to mature (complete, Figure 1) and hypermature (complete yet resorbing lens, with lens capsule wrinkling and crystalline refractive opacities present). Visual impairment can result from almost any stage of cataract (eg a small cataract in the axial, posterior lens capsule will be directly in the path of the most important central light rays), although obviously more complete cataracts elicit greater visual impairment.
In the dog, the most common cause of cataract is genetic predisposition, with over 90 breeds identified as predisposed. Other common causes of canine cataracts are diabetes mellitus, age (“senile” cataract), trauma, uveitis, glaucoma, progressive retinal atrophy, and lens luxation… in other words, any condition that affects the balance of aqueous humor flow to the lens can result in metabolic derangement of the lens protein fibers and thus cataract formation.
In diabetics, 50% of dogs will develop cataracts within 6 months of diagnosis, 75% within a year, and 80% within 16 months (Beam et al, 1999). It is therefore extremely important in this disease to educate clients, monitor the lens for cataract formation, and refer patients at an appropriate time. Generally, most veterinary ophthalmologists would prefer to be involved as early in the process as possible (upon diagnosis, or even before cataract diagnosis in the case of predisposing conditions such as diabetes). Since diabetic cataracts will often develop in the very periphery of the lens, they can be difficult to detect without iatrogenic dilation and careful slitlamp biomicroscopic evaluation.
When cataracts are developing, topical anti-inflammatory drops (such as non-steroidal diclofenac and flurbiprofen, or in more severe cases the steroids prednisolone acetate and dexamethasone) are recommended to reduce lens-induced uveitis, which can be the root cause of many other sequelae such as glaucoma and retinal detachment. Even if cataract surgery is not elected, lifelong topical anti-inflammatories should be continued. A recent retrospective review showed that “failure” (blindness, although euthanasia and deaths were also counted) of an eye was more likely in untreated eyes (8 of 8) than medically treated eyes (20 of 35, 57%). However, surgically treated eyes had the lowest failure rate (7 of 34, 21%). [Lim et al, 2011]
Surgical extraction of cataracts remains the gold standard approach, and is usually recommended when cataracts are immature, as the lens will be softer and easier to extract. Some will choose to wait, with careful monitoring, until the immature cataract is causing noticeable visual impairment, although adaptation to the home environment can mask the severity of impairment. Recent research, presented at the American College of Veterinary Ophthalmologists conference in 2012, into non-surgical options for diabetic cataracts suggests that the vision supplement Ocu-GLO may slow development (Williams & Colitz, 2012, Abstract #119). This is, however, only a preliminary and non-peer-reviewed finding. Meanwhile, a topical aldose reductase inhibitor has shown promise in reducing cataract formation in diabetics, by halting the enzyme pathway that leads to the osmotic gradient responsible for lens imbibition (Kador et al, 2010). When and if this drug, Kinostat™, receives FDA approval, the management of diabetic cataracts may be revolutionized. However, the cost and lifelong thrice daily frequency required for this drug may limit its clinical application, leaving cataract surgery as the more efficient approach to case management.
Prior to cataract extraction, a thorough assessment of the retina is made by the ophthalmologist. An electroretinogram (ERG) will show the functional activity of the retina (Figures 2 & 3).

Figure 2: Electroretinography being performed for a diabetic cataract; there is a contact lens electrode on the cornea, one visible subcutaneous electrode, and the light source (yellow probe).
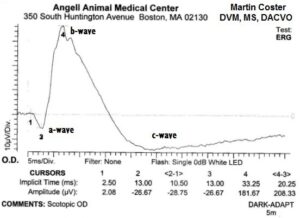
Figure 3: Electroretinogram tracing, showing a normal waveform. The amplitude of the b-wave (4-3; the greatest peak) was 208µV; generally any value greater than 100µV is considered healthy. This dog underwent successful cataract surgery.
Ocular ultrasonography is performed to confirm structural integrity of the retina, ruling out pre-existing retinal detachment (Figures 4 & 5). At Angell Animal Medical Center, ERG and ocular ultrasonography are performed under sedation.

Figure 4 – Ocular ultrasound of an eye with cataract (cornea is at the top of the image, retina at the bottom). The retina is not detached; this eye underwent successful cataract surgery.
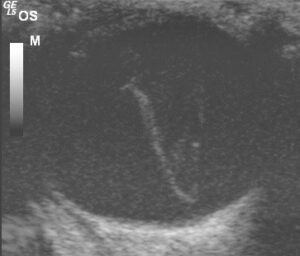
Figure 5 – Ocular ultrasound of an eye with retinal detachment (the retina is the V-shaped structure in the vitreous). This eye was not a candidate for surgery. (This oblique view of the globe does not clearly show the lens; the cornea is at the top of the image.)
In eyes with healthy retinas, cataract surgery can be elected. Modern cataract surgery uses an ultrasonic phacoemulsification probe to break up and extract the lens through a small ~3mm incision. An intraocular lens (IOL), made of acrylic, is then implanted in the majority of cases to improve focusing ability (for a video of a recent cataract surgery performed by Dr. Coster, click here). For a history of advances in cataract surgery, see Bellan, 2008, and for the development of IOLs by Sir Harold Ridley, Apple, 2006.
A recent advance in cataract surgery involves the treatment of lens subluxation with a surgical device called a Capsular Tension Ring (see here for a recent implant performed by Dr. Coster). Often, the decision to implant a CTR is made intraoperatively, and CTRs have allowed the placement of IOLs into eyes that otherwise would not have received them, improving functional vision.
Post-operatively, cataract surgery is generally considered to have an excellent success rate in vision restoration, typically 90-95% in the immediate post-operative period. Numerous peer-reviewed articles have examined the success and complication rates following phacoemulsification cataract surgery in the dog, and a summary is provided in Table 1. Additionally, the present author performed a meta-analysis on the available data from these studies, presented in Table 1.
| Year | 1987 | 1991 | 1996 | 2000 | 2001 | 2005 | 2006 | 2006 | 2011 | Weighted |
| Author | Miller | Davidson | Smith | Biros | Lannek | Johnstone | Sigle | Appel | Klein | Meta-Analysis |
| No. dogs | 56 | 182 | 88 | 220 | 154 | 143 | 172 | 108 | 103 | 1226 |
| No. eyes | 82 | 296 | 139 | 346 | 244 | 290 | 203 | 179 | 1779 | |
| Vision (%) | 71-94 | 95 | 87 | 80-95 | 92 | 83 | 86% | |||
| POH (%) | 38 | 49 | 34 | 23 | 25% | |||||
| Uveitis (%) | 15 | 8 | 16 | 9% | ||||||
| PCO (%) | 11 | 65 | 69 | 60% | ||||||
| Glaucoma (%) | 4.8 | 3 | 16.8 | 14 | 11 | 12.4 | 6.7 | 11% | ||
| RD (%) | 4.8 | 4.7 | 3 | 1-2 | 8.4 | 4% | ||||
| Bleeding (%) | 2 | 2 | 12 | 5% | ||||||
| Corneal Opacity (%) | 29 | 2 | 19 | 9.5% |
Table 1: Summary of 9 major reviews of success and complication rates following phacoemulsification cataract surgery in the dog. Blank spaces indicate data were not available in the published article. Weighted meta-analysis was performed by the present author on available data. POH, Post-operative ocular hypertension; PCO, posterior capsular opacification; RD, retinal detachment.
Glaucoma and retinal detachment are the most significant potential post-operative complications, due to ensuing blindness. Post-operative ocular hypertension is generally a transient and treatable increase in pressure of the eye, and is the reason we hospitalize our patients at Angell, for overnight monitoring following surgery. The reported uveitis rate refers to clinically significant uveitis, as the large majority of cataract patients will have post-operative inflammation to some extent.
Posterior capsular opacification (“after cataract”) of the remnant lens capsule is a very common phenomenon, but is rarely clinically significant in this author’s opinion. Intraocular hemorrhage and corneal opacification are of variable significance.
In a study of client satisfaction following cataract surgery (Appel et al, 2006), at 12 months follow-up, 81% of owners were satisfied with their decision to pursue surgery (whereas 95% of evaluating clinicians were satisfied with the dog’s visual outcome). Dissatisfaction reasons included vision loss as assessed by the owner (8%), diabetic control (3%), perceived poor value for money (1%), and unrelated neoplastic processes (2%). “Dissatisfied owners were significantly more likely to report that explanation of risks and complications before surgery was inadequate.” However, dissatisfied owners also did not return for follow-up, which is an essential component of success.
In conclusion, cataract surgery is an elective procedure that offers a high rate of success in restoring vision to compromised eyes. Involvement of an ophthalmologist as early as possible in the process of cataractogenesis is recommended, so that adequate client education, monitoring, and timely medical and surgical intervention can be performed, maximizing success.
For more information about Angell’s Ophthalmology service, please visit www.angell.org/eyes. Drs. Coster and Biros are available for consults or referrals at 617-541-5095, or e-mail ophthalmology@angell.org
