-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 By Jessica Riehl, DVM, DVDC
By Jessica Riehl, DVM, DVDC ![]()
angell.org/dentistry
dentistry@angell.org
617-522-7282
August 2025
X
Introduction
Dogs and cats often present for dentistry services due to routine periodontal disease, endodontic infection, and tooth resorption. However, another cause for presentation can include jaw fractures. The most common cause of jaw fractures is trauma such as bite injuries, being hit by a car, blunt force trauma, or falls. Jaw fractures can also occur secondary to iatrogenic reasons (surgical complications +/- pathology involved) or primary pathologic cause due to tumor or severe periodontal bone loss.
For bone fracture healing to occur, the area must undergo a similar process to soft tissue healing with phases of inflammation, removal of organic debris, cellular proliferation, and formation of granulation tissue. In the presence of necrotic bone, osteogenic precursor cells must transform the granulation tissue into callus and eventually into bone. There are two types of healing for bone fractures: either indirect or direct bone healing. In indirect healing, mechanical instability of the fracture, resorption of the fracture ends, and callus formation occur. In contrast to direct bone healing, there is close apposition of the fracture segments and mechanical stability, which allows the fracture ends to make direct contact and bridging of the bone.
Further breakdown of direct bone healing can be categorized into contact healing and gap healing. Direct bone healing occurs when there is anatomic reduction and absolute rigid fixation. In this situation, bone is the only type of connective tissue to form between the fracture segments during healing. Here, there is a quicker function and none of the potential consequences that can occur with large callus formation.
Indirect bone healing begins with the inflammatory phase of fracture repair, which occurs as a result of ruptured blood vessels and a torn periosteum. Ischemic necrosis of the bone ends occurs a few millimeters from the ends of the fracture segments. Osteogenic cells will be activated, and a vascular response will begin. Fibroblast proliferation occurs in the blood clot, and a cellular infiltrate with neutrophils and macrophages accumulates. The debris in the fracture region will be removed by these cells. Additional fibroblasts, chondroblasts, osteoblasts, and osteoclasts will result from differentiation. The proliferating cells then form a callus, a fibrous matrix of collagen that bridges the fracture segments. Granulation tissue replaces the initial hematoma, and during the reparative phase, the callus matures. Fibrocartilage will form and eventually undergo mineralization. Endochondral ossification will then replace this with bone, resulting in a healed fracture. For both fracture types, an increase in strength will occur as the bone remodels and returns to its original shape. Woven bone is replaced with lamellar bone in this process.
Although the mandible does not have a medullary canal, it heals similarly to other long bones. The bones of the maxilla and face, however, have a thin lamina and greater bone surface area per unit volume exposed to soft tissues. The facial bones thus have increased proximity to the vascular supply of the soft tissues, which is beneficial for rapid bone healing. A major difference in healing between maxillofacial fracture healing versus long bones is the presence of teeth and the mandibular canal. The teeth make fixation more challenging as they occupy a large volume of the mandible and can create difficulty with applying rigid stabilization along the tension-band side of the bone, where biomechanics dictate the preferred placement of implants. The dorsal 2/3 of the mandible is occupied by the tooth roots, and the ventral 1/3 houses the mandibular canal. Additionally, in comparison to humans, the dorsoventral mandibular height is drastically more limited. Our pet patients have a larger tooth root volume compared to humans, which limits the surfaces available for implant placement.
One of the primary surgical goals for repairing maxillofacial and mandibular fractures in patients is to restore proper dental occlusion. In restoring normal occlusion, this subsequently ensures appropriate fracture reduction. If this is not achieved, the resulting malocclusion can adversely affect function and can also cause undesirable leverage forces against the fixation device.
When considering mandibular fractures, there are two general categories: favorable and unfavorable fractures. This is based on the direction of the fracture line, where favorable fractures run from dorsocaudal to ventrocranial. Conversely, unfavorable fractures progress from dorsocranial to ventrocaudal. The concept is derived from the forces the muscles of mastication apply to the mandible. The masseter, temporal, and medial pterygoid muscles are responsible for closing the mouth in the normal situation. They will also “lift” the caudal mandible, where the muscles insert on the body of the mandible and ramus. On the other hand, the small digastricus muscle, with its insertion on the angle of the mandible, is responsible for opening the mouth. Thus, in favorable fractures, the muscles of mastication compress the fracture segments together and “assist” with bony healing. In unfavorable fractures, the masticatory muscles cause distraction of the fracture segments.
Maxillary fractures may not require stabilization because, in the maxilla, forces exerted on the upper jaw are different compared to the mandible, and the maxilla is subject to less strain. There is a “frame” or “box” structure that provides anatomic buttresses and distributes masticatory forces to the head. Maxillary fractures may not require stabilization unless the buttresses are disrupted.
If fractures are not properly fixed, maxillofacial fractures can result in cavitation, associated soft tissue complications, delayed or non-union healing, and sequestrum formation, in addition to contracture of fibrous connective tissue, which can lead to deformities. Restoring normal anatomy can alleviate pain and discomfort and permit more rapid healing.
Methods for Fracture Repair
Fracture repair can involve various techniques. For simple separation of the mandibular symphysis or parasymphyseal fractures, cerclage wire placed around the rostral mandible caudal to the canine teeth is often the simplest method of stabilization. Another technique that can be performed is to place an interdental wire and composite resin as a splint spanning from one canine tooth to the contralateral side.
Intraoral Splints
For other fractures in the body of the mandible or involving the maxilla, interdental wiring and composite resin splints are often the least invasive fracture repair technique, as they do not require exposure of the bone or disruption to the periosteum. They can allow normal function and masticatory forces after placement. This technique can involve either forms of cerclage wiring or interdental wiring along with self-hardening composite resin, which can be bonded to the teeth. The composite resin adds additional strength to the splint and covers any sharp wire twists.
Interdental wire can be placed with several patterns, which are indicated by fracture location and operator preference. The wire is anchored around and between the crowns of the teeth, utilizing the teeth as anchor points and allowing for fracture fragment alignment and fixation. Following the placement of the wire, a portion of the tooth surface is treated with an acid etchant and a bonding agent to ensure that the composite material adheres. Some materials can be used without the need for bonding agents, and familiarity with the products being used is crucial. This combination of integrating interdental wiring and a composite splint increases the strength of the splint, similar to how rebar reinforces a concrete structure, helping it withstand bending, cracking, or other forces. The use of both interdental wiring and composite splinting has been shown to be more effective than either method alone.
Once fracture healing has occurred, the splint is removed by sectioning the composite resin, transecting the wire, and removing the splint in segments. Maintaining as many healthy teeth as possible is crucial for intraoral splinting, as these are part of the fracture stabilization method. A splint will ideally incorporate at least two to three teeth rostral and two to three teeth caudal to the fracture line. Teeth compromised by severe periodontal disease are not useful for intraoral splinting. Thus, intraoral splinting will be best when there are periodontally sound teeth, a lack of a bony defect, and minimal comminution of the fracture.
Intraosseous Wiring
Intraosseous wiring can be beneficial to use as a small implant in situations where other types of fixation, such as plating, are too large or difficult to apply. The wires placed aim to draw the fracture segments together, resulting in dynamic compression that brings the bone into proximity, allowing for healing. This technique requires that fractures are simple (non-comminuted), the segments interdigitate well, and the nature of the fracture itself is relatively stable. Intraosseous wiring should not be used in fractures where there are gaps or comminution of the fracture fragments. Although the use of intraosseous wiring draws the fracture segments to one another, the bone can still have rotational force because, naturally, the pilot holes in the bone will be slightly larger in diameter than the wire itself. Two regions of fixation are preferred to prevent torsion and shearing forces. The more dorsal of the wires should be placed close to the alveolar margin, where tensile stress is natural in the mandible, and ideally perpendicular to the fracture line. To avoid damaging tooth roots, pilot holes can be placed between teeth or in the furcational bone. The second stabilization wire can be placed parallel to the ventral margin of the mandible. The wires will often become covered with bone and can remain in place. However, if the wires become loose or erosion of the oral mucosa over the wires occurs, the wire should be removed.
Plating
For plating techniques, miniplates and locking plates are used due to their small size. The benefit of plating fractures is that with appropriate use, the rigid fixation can create anatomic realignment and permit primary bone healing.
The mandible will require two plates, utilizing a tension-band principle, where one plate is positioned near the alveolar margin and the second plate helps to neutralize shearing or torsional forces further. The plates should be placed parallel to one another. Plate fixation can be more difficult in smaller breeds of dogs, where the tooth root:mandible height ratio is greater than in larger breeds. Sometimes in these cases, a single large plate along the buccal aspect of the ventral mandible may be reasonable. Penetration of tooth roots will result in damage to the vascular supply of the tooth and eventual pulp necrosis and therefore should be avoided. A penetrating screw into a tooth can create bacterial access to the tooth and eventual endodontic disease. A combination of techniques can be used if placement of a plate along the alveolar margin is not feasible; an intraosseous or interdental wire can be used.
Significant defects may be present in certain fractures, and for these, a bridging plate can provide stability in combination with either cancellous bone grafting or a cortical bone graft. Cancellous grafts can stimulate bone healing in the presence of gaps or comminuted fractures. The cortical bone graft acts as a strut and can share some of the support of the fixation device. For placement of the plate, there should be at least three screws on each side of the fracture. Repair using plates can be difficult in regions where the bone is very thin, such as the maxilla and mandibular ramus. Screw length is crucial to prevent perforation of the oral mucosa, which can lead to infection or further trauma to intraoral soft tissues. Referral to a University is often recommended if mini plating is desired for severe maxillofacial injuries.
Maxillomandibular Fixation
Maxillomandibular fixation (MMF) involves connecting the maxillary and mandibular arcades with columns of composite spanning between the maxillary canine teeth to the mandibular canine teeth. This form of interdental bonding enables the alignment of occlusion and the stabilization of the jaw. Still, it is not suitable for cases where there are gap defects or comminution of the fracture. Generally, this procedure is reserved for fractures caudal to the regions of the jaw containing teeth or for injury to the TMJ. These patients may be able to lap up gruel, but esophagostomy tube placement should be performed before interdental bonding. Care must be taken to consider the time frame during which a patient is placed on MMF to prevent functional ankylosis of the temporomandibular joint.
A modified technique of MMF using labial buttons and sutures can keep the mouth in a mostly closed position while still permitting some movement of the TMJ. This reduces some of the risk of functional ankylosis, although it still requires consideration of the duration of treatment.
Muzzle Coaptation
The nylon muzzle and tape muzzles serve to limit the mouth opening and maintain the pet’s occlusion while also providing support to the ventral mandible as a sling. This is the least invasive method for jaw fracture treatment, but it will have the most significant risk for healing complications, most notably malocclusion. When using a form of muzzle as a coaptation, the technique must ensure that the crowns of the canine teeth overlap by 30% to 50% of the crown height, thereby maintaining interdigitation of the teeth and ensuring they remain in occlusion.
Mandibulectomy or Maxillectomy
Partial jaw excision is a last resort or salvage procedure to address particular situations where there is poor quality or quantity of bone to permit healing, or financial constraints prevent consideration of surgical repair. These procedures remove a fractured segment of the jaw to avoid bone-to-bone contact and the associated pain that is related to this. These procedures often result in a malocclusion, particularly in the mandible, where mandibular drift can occur.
Conservative techniques for non-invasive fracture management can range from tape muzzles to nylon muzzles to interdental wire and composite splints. These non-invasive techniques will reduce the risk of iatrogenic trauma to the tooth roots and neurovascular structures of the mandible. They will avoid disruption to the fracture hematoma, eliminate surgical trauma to the periosteum, and decrease the risk of additional bacterial contamination at the fracture site.
Disadvantages of non-invasive techniques include difficulty with reduction and apposition, as these techniques create a semirigid fixation that allows for micromotion. The non-invasive methods are not the primary choice for severely comminuted or unstable fractures. Often, non-invasive techniques are preferred for young patients, particularly those with deciduous or mixed dentition, as plating can cause damage to developing tooth buds, and exposure of the periosteum may interfere with skeletal growth. Edentulous patients can consider the placement of an intraoral splint and cerclaging to the mandible; however, open reduction and internal fixation may be a better treatment option. Non-rigid muzzle coadaptation and MMF can lead to delayed healing, excessive callus formation, and non-healing.
The decision on whether a tooth is involved in the fracture line and whether extraction of the tooth is required can also influence the decision-making process for the fracture repair method. Previous studies have demonstrated, for example, that the presence of the first molar tooth in canine mandibular fractures affects the strength of an intraoral splint. Regardless of the technique used for fracture repair, teeth at the fracture line or rostral to the fracture line should be assessed in six to 12 months to ensure they remain vital, as the blood supply may have been compromised at the time of injury.

Figure 1. Three-dimensional image produced from a CT scan demonstrating a favorable fracture of the right caudal mandible in a canine patient. This fracture was a result of a dog bite injury.

Figure 2. Same patient as Figure 1. Three-dimensional image produced from a CT scan. Lingual view of fracture.

Figure 3. Same patient as Figures 1 and 2. Three-dimensional image produced from a CT scan. Ventral view.

Figure 4 (A + B). Same patient as Figures 1, 2, and 3. Dental radiographs of mandibular fracture at the level of the mandibular first molar (409). The injury involves a fracture of the distal root of the tooth as well as a disruption of the bone at the apical region of the mesial root. There is a periodontal disease associated with the second molar (410) unrelated to the injury.
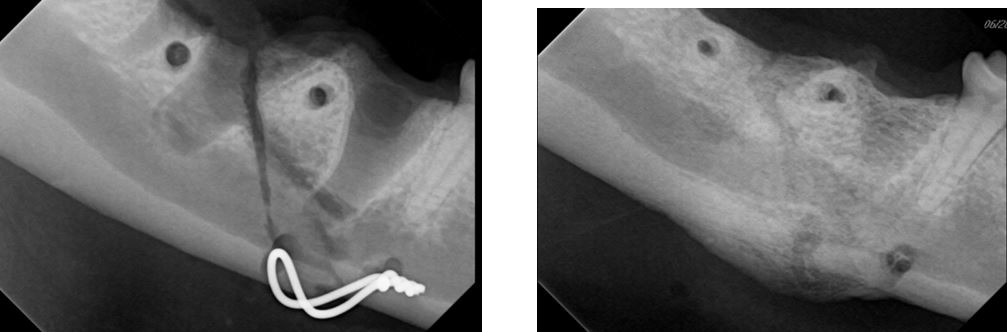
Figure 5 (A + B). Same patient as Figures 1, 2, 3, and 4. Figure A shows the intraoperative placement of an intraosseous wire. Pilot holes have been created for the dorsal wire, aiming for wire positioning that is approximately perpendicular to the fracture line. The ventral wire is in a “figure 8” on the ventral aspect of the mandible. Figure B is two months after fracture repair, and intraosseous wires are removed. Union between the bone segments is present, along with callus formation along the ventral mandible.

Figure 6. Intraoral view of an anesthetized feline patient that suffered unwitnessed trauma (fall or crushing injury). Note soft tissue trauma in the symphyseal region and bruising lingual to the left mandible.

Figure 7. Same patient as Figure 6. Dental radiograph of the left mandible with a favorable fracture. Fracture has disrupted the bone around both apices of the molar tooth (309).

Figure 8 (A + B). Same patient as Figures 6 and 7. Demonstrating fixation techniques for mandibular fracture and symphyseal separation. Two cerclage wires were placed around the left mandible along the oblique fracture. An intraoral technique for symphyseal wiring was performed with a wire twist located intraorally distal to the left mandibular canine tooth (304). A bead of composite was placed over the wire twists to prevent trauma to soft tissues.

Figure 9. Same patient as Figures 6, 7, and 8. An esophagostomy feeding tube is in place to facilitate feeding. Modified labial button technique performed to limit movement of the mouth in the short term to support healing. The buttons and suture can be removed on a compliant conscious patient (+/- pre-visit sedation) or after receiving injectable sedation in the hospital.

Figure 10. Same patient as Figures 6, 7, 8, and 9. Presenting two months post-fracture repair. Symphyseal wire with composite bead is visible distal to the mandibular canine tooth (304). The rostral cerclage wire around the mandible between the third and fourth premolars (307, 308) is visible. Not in view is the cerclage wire caudal to the molar (309).

Figure 11 (A + B). Same patient as Figures 6, 7, 8, 9, and 10. Follow-up eight months later, at which time the mandibular molar (309) was extracted due to initial damage to the apical blood supply to this tooth. The tooth was not extracted at the two-month visit when the wires were removed to avoid iatrogenic damage to the recently healed fracture. Root canal therapy was performed two months post-fracture, when the wires were removed due to pulp exposure resulting from the initial injury. A well-healed fracture and symphysis are present.

Figure 12. Dental radiograph of a canine patient with a fracture of the left rostral mandible and extrusive luxation of the left mandibular canine tooth (304).

Figure 13 (A + B). Same patient as Figure 12. Intraoral splint comprised of interdental wire and composite resin placed following the extraction of the left mandibular incisors (301, 302, 303) and the reimplantation of the luxated canine tooth (304).
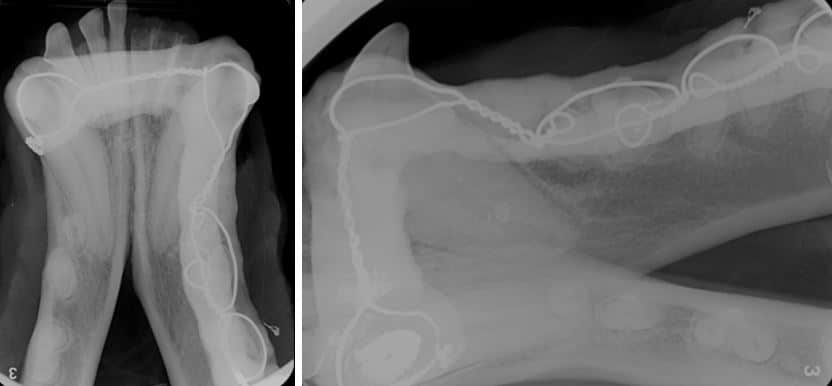
Figure 14 (A + B). Same patient as Figures 12 and 13. Dental radiographs two months following fracture repair. Interdental wiring and composite splint before removal. The previously luxated canine tooth was treated with root canal therapy at this visit, following splint removal.
References
- Lothamer C, Snyder CJ, Duenwald-Kuehl S, Kloke J, McCabe RP, Vanderby R Jr. Crown Preservation of the Mandibular First Molar Tooth Impacts the Strength and Stiffness of Three Non-Invasive Jaw Fracture Repair Constructs in Dogs. Front Vet Sci. 2015 Jul 17;2:18.
- Scherer E, Hetzel S, Snyder CJ. Assessment of the Role of the Mandibular First Molar Tooth in Mandibular Fracture Patterns of 29 Dogs. J Vet Dent. 2019 Mar;36(1):32-39.
- Snyder CJ, Bleedorn JA, Soukup JW. Successful Treatment of Mandibular Nonunion With Cortical Allograft, Cancellous Autograft, and Locking Titanium Miniplates in a Dog. J Vet Dent. 2016 Sep;33(3):160-169.
- Soukup JW, Snyder CJ. Transmylohyoid orotracheal intubation in surgical management of canine maxillofacial fractures: an alternative to pharyngotomy endotracheal intubation. Vet Surg. 2015 May;44(4):432-6.
- Boudrieau RJ, Kudisch M. Miniplate fixation for repair of mandibular and maxillary fractures in 15 dogs and 3 cats. Vet Surg. 1996 Jul-Aug;25(4):277-91.
- Guzu M, Hennet PR. Mandibular body fracture repair with wire-reinforced interdental composite splint in small dogs. Vet Surg. 2017 Nov;46(8):1068-1077.
- Castejon-Gonzalez AC, Reiter AM. Dental Abnormalities in Immature Dogs with a History of Mandibular Fractures. J Vet Dent. 2022 Jun;39(2):173-181.
- Castejón-González AC, Stefanovski D, Reiter AM. Etiology, Clinical Presentation, and Outcome of Mandibular Fractures in Immature Dogs Treated with non-Invasive or Minimally Invasive Techniques. J Vet Dent. 2022 Mar;39(1):78-88.
- Legendre L. Intraoral acrylic splints for maxillofacial fracture repair. J Vet Dent. 2003 Jun;20(2):70-8
- Pakula J, Freeman A, Perry A. Clinical outcomes of mandibular body fracture management using wire-reinforced intraoral composite splints in 15 cats. Front Vet Sci. 2025 Mar 24;12:1552682.
- Verstraete, Frank J. M., et al. Oral and Maxillofacial Surgery in Dogs and Cats. Second edition