-
Adopt
-
Veterinary Care
Services
Client Information
- What to Expect – Angell Boston
- Client Rights and Responsibilities
- Payments / Financial Assistance
- Pharmacy
- Client Policies
- Our Doctors
- Grief Support / Counseling
- Directions and Parking
- Helpful “How-to” Pet Care
Online Payments
Emergency: Boston
Emergency: Waltham
Poison Control Hotline
-
Programs & Resources
- Careers
-
Donate Now
 By Brooke Simon, DVM
By Brooke Simon, DVM![]()
angell.org/dermatology
dermatology@angell.org
617 524 5733
Introduction
Primary secretory otitis media (commonly abbreviated as PSOM) is a relatively uncommon disease that has been reported primarily in Cavalier King Charles spaniels. Very few other reports have been noted in breeds outside the Cavaliers, and unfortunately the breed predilection is unknown.
Pathogenesis
 Pathogenesis of PSOM is unfortunately unknown as well. The theories that have been postulated include that either an increase in production of mucus, decreased drainage of the middle ear through the Eustachian tube, or a combination of both are contributing factors. In human patients, chronic drainage of the tympanic cavity occurs through the Eustachian tube; if we assume that this is a similar pathomechanism in our canine patients, there is likely an impaired patency of the Eustachian tube and tympanic cavitary mucociliary clearance that is compromised in cases of PSOM.
Pathogenesis of PSOM is unfortunately unknown as well. The theories that have been postulated include that either an increase in production of mucus, decreased drainage of the middle ear through the Eustachian tube, or a combination of both are contributing factors. In human patients, chronic drainage of the tympanic cavity occurs through the Eustachian tube; if we assume that this is a similar pathomechanism in our canine patients, there is likely an impaired patency of the Eustachian tube and tympanic cavitary mucociliary clearance that is compromised in cases of PSOM.
Clinical Signs
The primary presenting complaint in this author’s experience is gradual hearing loss that can occur over a 3-8 month period, sometimes concurrently with head shaking/ear irritation with no evidence of concurrent otitis externa.
In other cases, pain can be localized to the head/neck with spontaneous episodes of neck guarding. Intense pruritus affecting the pinna and/or external ear canals (with no concurrent otitis externa), head tilt, nystagmus, ataxia, facial nerve paralysis, fatigue, and varying degrees of otitis externa can also be seen.
Diagnosis
Diagnosis of PSOM is dependent on signalment, clinical signs, and clinical findings. Otoscopic examination in a PSOM patient should reveal a bulging pars flaccida and pars tensa, however a normal appearance to the tympanic membrane does not rule out PSOM. In many cases, if one tympanic membrane appears affected on otoscopy however the other appears overtly normal, there will be some level of disease still present in the normal-appearing side as well (bilateral in approximately 60% of cases according to one study).
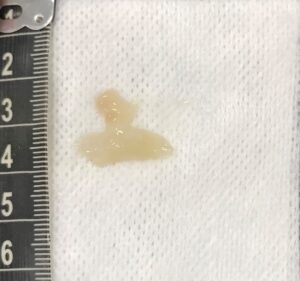
An example of the discharge flushed from the bulla after a myringotomy has been performed in a PSOM-affected patient.
Diagnostic imaging with either radiography or computer tomography (CT is preferred) of the bulla should reveal changes consistent with effusion of the middle ear, with or without concurrent osteitis.
Definitive diagnosis is achieved after myringotomy to reveal a typically viscous, opaque, grey to yellow plug of mucous present in the bulla.
Treatment
The primary treatment recommendations in a symptomatic patient affected with PSOM is removal of the plug of mucous in the tympanic cavity through a myringotomy incision. Repeated myringotomies/bulla flushings have been required in some cases due to the healing of the myringotomy site and continued accumulation of mucoid discharge in the bulla over time.
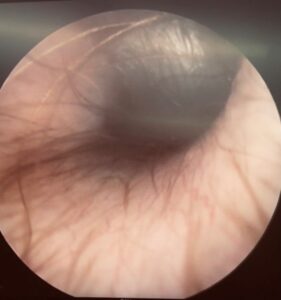
Photograph of a visible bulging pars tensa component of the tympanic membrane on video otoscopy. Note the hairs extending from the base of the tympanic membrane, and “shiny” appearance of the distended pars tensa.
Pharmacological intervention in some PSOM cases has not been fully explored, including mucolytics and leukotriene inhibitors which appear to be ineffective. However pharmacological interventions have largely been unrewarding in this disease process.
A few studies have been performed to assess whether tympanostomy tubes (as those used in human medicine) provided enough continued tympanic cavity ventilation and drainage.
Post-operative medications have included corticosteroids (both topical and systemic), antibiotics, and in some cases a mucolytic (acetylcysteine or bromhexine).
Recurrence of PSOM is common, with one study reporting almost 20% of dogs having relapses of clinical PSOM 6-18 months after their first procedure.
Reference
- Stern-Bertholz W, Sjostrom L, Hakanson, NW. Primary secretory otitis media in the Cavalier King Charles spaniel: a review of 61 cases. Journal of Small Animal Practice 2003; 253-256.
- Cox CL, Slack RWT, Cox GJ. Insertion of a transtympanic ventilation tube for the treatment of otitis media with effusion. Journal of Small Animal Practice 1989: 30; 517-519.
- Corfield GS, Burrows AK, Imani P, et al. The method of application and short term results of tympanostomy tubes for the treatment of primary secretory otitis media in three Cavalier King Charles Spaniel dogs. Australian Veterinary Journal 2008; 86: 88-94.
- Cole, L. Primary Secretory Otitis Media in Cavalier King Charles Spaniels. Vet Clin Small Anim 2012; 42: 1137-1142.
- Burrows, M. Primary secretory otitis media (PSOM) of Cavalier King Charles spaniels. ACVS proceedings. 2008.
- Miller W., Griffin C, Campbell K. Small Animal Dermatology 7th St. Louis, Elsevier, 2013.